- Visibility 223 Views
- Downloads 51 Downloads
- Permissions
- DOI 10.18231/j.jsas.2020.013
-
CrossMark
- Citation
Depression and its Dilemma
- Author Details:
-
Sunil Chaudhry *
Abstract
Depression is a common mental disorder that presents with depressed mood, loss of interest or pleasure, decreased energy, feelings of guilt or low self-worth, disturbed sleep or appetite, and poor concentration. Depression shall become the second largest illness in terms of morbidity by another decade. 50-65% of patients respond to the first antidepressant. No particular antidepressant agent is superior to another in efficacy or time to response. Depression is less prevalent among older adults than among younger adults but can have serious consequences. Choice can be guided by matching patients’ symptoms to side effect profile, presence of medical and psychiatric co morbidity. The adequate treatment of residual symptoms following an acute depressive episode, including insomnia symptoms, may prevent relapse. In the near future, developments are likely to remain focused on monoamine neurotransmitters, with the aim of finding agents that are either more effective, better tolerated or that have a faster onset of action than existing options.
Introduction
Definition
Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems.
Depression symptoms can vary from mild to severe and can include: ICD[1] 10 Guidelines for diagnosing depressive episode [[Table 1]] [2], [3].
|
Typical Symptoms |
Other Symptoms |
|
|
Depressed mood |
Reduced concentration and attention |
Mild Depressive episode: atleast 2 typical symptoms and 3 or 4 other symptoms |
|
Loss of interest / enjoyable of activities that are normally pleasurable |
Reduced self esteem and self confidence |
Moderate Depressive Episode : atleast 2 typical symptoms and 3 or 4 other symptoms |
|
Decreased energy or increased fatigue |
Ideas of guilt and unworthiness |
Severe Depressive Episode: All 3 typical symptoms & other 4 symptoms |
|
|
Bleak and pessimistic view of future |
|
|
|
Ideas of acts of self harm or suicide |
|
|
|
Disturbed sleep & appetite |
|
The report on Global Burden of Disease estimates the point prevalence of unipolar depressive episodes to be 1.9% for men and 3.2% for women, and the one-year prevalence has been estimated to be 5.8% for men and 9.5% for women. It is estimated that by the year 2020 if current trends for demographic and epidemiological transition continue, the burden of depression will increase to 5.7%. 7% of the population had at least one major depressive episode in one year. The prevalence of depression in community samples and the prevalence rates have varied from 1.7 to 74 per thousand population. Women and Elderly are more prone to get depression. [4]
Causes of Depression
Genetic
The genetic risk of developing clinical depression is about 40% if a biological parent. Genetic deletion of NMDA (n methyl d aspartate) receptor ε4 subunit.
DNA methylation is the best-characterized epigenetic modification. It seems that promoter-specific DNA methylation is correlated with gene silencing, but gene body (nonpromoter) DNA methylation correlates with increased gene activity.
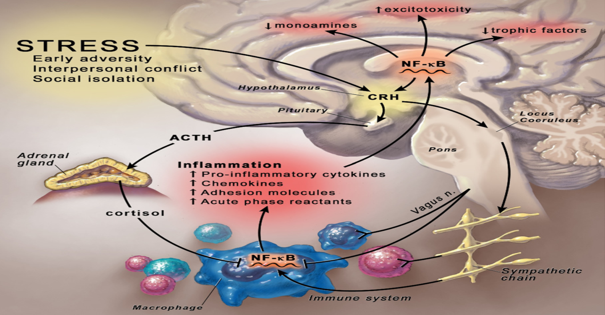
Immunological
Substantial evidence suggests that sustained activation of the immune system or chronic inflammation may be one of the underlying pathologic processes in depression. Elevated levels of proinflammatory cytokines such as interleukin 6 (IL-6), interleukin 1 (IL-1), tumor necrosis factor–alpha (TNF-alpha), interferon-gamma, as well as C-reactive protein (CRP, an acute phase protein) are consistently reported in depressed patients. Peripheral inducers of immune cytokines may generate symptoms of depression and in the brain, these inducers may decrease monoamine levels that most current antidepressants aim to increase.
Biochemical
Low concentrations of the major metabolite of 5HT (5-hydroxyindole acetic acid) are found in the CSF of patients who are depressed and suicidal. Elevated levels of serotonin contribute to the antidepressant effect.
Low levels of NE metabolites are found in the urine and CSF of depressed patients. Depletion of NE in depressed patients in remission treated with a NE reuptake inhibitor precipitates a relapse in depressive symptoms. A blunted growth hormone response to the D2 adrenergic agonist clonidine is found in depressed patients.Increased density of B-adrenergic receptors is found in postmortem brain tissue in the cortex of depressed suicide victims.Increased. MAO-A activity is found in the CNS of depressed patients.
Hyperactivity of HPA axis is one of the commonest neurobiological changes in depressive patients (dysfunction of HPA axis is manifested in about 70% patients of depression. corticotrophin releasing factor (CRF). Subsequently, CRF enters the hypothalamic portal venous system and stimulates the corticotrophs located at the anterior pituitary gland to synthesize proopiomelanocortin (POMC), This stimulates release of ACTH. Upon activation of HPA axis by the psychological stress, more GCs are released into the blood. Concentrations of vasopressin were elevated in depressive patients which might conduce to the hyperactivity of the HPA axis in those patients
The levels of glutamate (or glutamine) in patients with depression were found elevated in the brain, cerebrospinal fluid and plasma. There is a hypothesis that the activation of the GABA receptors may produce antidepressant effects. [[Figure 1]]
Drug and alcohol abuse
Approximately 30% of people with substance abuse problems also have depression.
Medical conditions
People who have a history of sleep disturbances, medicalillness, chronic pain, anxiety, and attention-deficit hyperactivity disorder (ADHD) are morelikely to develop depression.
Trauma
When people experience trauma at an early age, it can cause long-term changesin how their brains respond to fear and stress.
Cancer
Depression remains an under-recognised comorbidity in cancer patients, with major implications on patient suffering, mortality and healthcare expenditure. Treatment of depression in patients with cancer can enhance quality of life.
Life circumstances
Marital status, financial standing where these play vital role.
Post partum depression
Affects 50-80 % of new mother. Symptoms begin usually 3-4 days after delivery, worsen by day 5-7 and tends to taper by day 12. [5], [6], [7]
Types of Depression
Major depressive disorder
Symptoms on most days for 2 weeks or longer. Overall, between 20% and 25% of adults may suffer an episode of major depression at some point during their lifetime. Twice as many women as men have major or clinical depression; hormonal changes during puberty, menstruation, pregnancy, miscarriage, and menopause, may increase the risk.
Depression (dysthymia) that lasts for 2 years or longer, it's called persistent depressive disorder.
Bipolar Disorder
A disorder associated with episodes of mood swings ranging from depressive lows to manic highs.
Seasonal Affective disorder: which happens in winter or as season changes.
Psychotic depression
Depression along with Psychosis- Hallucinations, Delusions, Paranoia
Situational
Any trauma in Life such as accident or death of close relation
Atypical
Increased appetite, Sleeping more than usual, Feeling of heaviness in arms and legs, Oversensitive to criticism.
Peripartum (Postpartum) Depression and Premenstrual Dysphoric Disorder (PMDD) are not uncommon in women. [8]
Diagnosing Depression
The DSM 5 criteria for depression mentions physical fatigue and loss of energy. Depressed mood has to do with sadness or negative emotions. Anhedonia is loss of interest.
Patient Health Questionnaire (PHQ-9) is a 9-item self-report questionnaire that can assist in the detection of depression and supplement a thorough psychiatric and mental health status assessment.
Columbia Suicide Severity Rating Scale (C-SSRS) It can be used to assess severity of and trackchanges over times in suicidal ideation and behaviour.
Edinburgh Postnatal Depression Scale (EDPS) This 10-item self-report measure is designed to screen women for symptoms of emotional distress during pregnancy and the postnatal period. [9]
|
Monoamine reuptake inhibitors |
Tricyclic antidepressants: imipramine, amitriptyline, cloimipramine, lofepramine, amoxapine |
|
|
Noradrenaline reuptake inhibitors: desipramine, nortriptyline, maprotiline |
|
Selective serotonin reuptake inhibitors |
Flouxetine, Fluvoxamine, Zimeldine, Paroxetine, Sertraline, Citalopram, Escitalopram |
|
Non selective Monoamine oxidase inhibitors |
Phenelzine, Tranylcypromine, isocarboxazid |
|
MAO A inhibitors |
Mocloblemide , Toloxatone |
|
Serotonin NE reuptake inhibitors |
Venlafaxine, Duloxetine |
|
NE, DA reuptake inhibitors |
Nomifensine, Bupropion |
|
NE and selective serotonin antagonists |
Mirtazapine |
|
Serotonin antagonist and reuptake inhibitor |
Trazodone |
|
Serotonin partial agonist |
Gepirone |
|
5HTC receptor antagonist and melatonin receptor agonist |
Agomelatine |
No single antidepressant medication has been found to be the best treatment for every patient. In general 40% to 60% of patients will have a positive response to the first antidepressant medication they try. Second generation antidepressants (i.e., selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors [SNRIs]) are used preferentially over first generation antidepressants (i.e., tricyclic antidepressants [TCAs] or monoamine oxidase inhibitors [MAOIs]) because of a less toxic side effect profile and better patient tolerability. Typically, it takes from 4 to 8 weeks to have a full clinical response to an antidepressant.[10]
Mechanism of Antidepressants
The TCAs (Tricyclic antidepressants) block the reuptake of both norepinephrine (NE) and serotonin (5HT). This phenomenon being the primary mechanism of actions of antidepressants brings changes in the physiological behaviour of neuro-receptors. TCAs have also been reported to block muscarinic, alpha1 adrenergic and histaminic receptors. Selective serotonin-reuptake inhibitors (SSRIs) may block the reuptake of 5HT and increase. synaptic 5HT transmission. The activity of serotonin nor-epinephrine reuptake inhibitors (SNRIs) does not exert any side effects such as sedation or hypotension but display TCAs like activity. Higher doses of SNRIs have been reported to mildly increase blood pressure
Unlike tricyclic antidepressants, MAO inhibitors increase the levels of all three neurotransmitters, dopamine, norepinephrine and serotonin, in the brain and thereby regulate different aspects of behaviour, cognition, motivation, and mood [Figure 2[Figure 2] ]
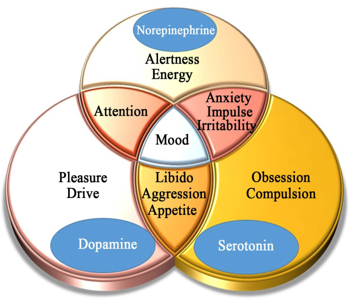
Antidepressants showing α-2 antagonism plus serotonin-2 and serotonin-3 antagonism - Mirtazapin Similar to nefazodone, mirtazapine also does not exert any toxicity of SSRIs due to 5-HT2 stimulation.The antidepressants acting as a noradrenaline specific reuptake inhibitor (NRI) (Reboxetine). Antidepressants as a serotonin reuptake enhancer (Tianeptine). Bupropion is the only antidepressant that selectively acts on the noradrenergic and dopaminergic systems and not on the serotonin system [1]
Herbal Drugs
Phytochemicals are reported to act as antidepressants. These chemicals present in the plant extracts are expected to be safer. Hypericum perforatum commonly known as St. John’s wort is the only herbal antidepressant that has been approved for the clinical management of mild to moderate cases of depression. Hypericin and hyperforin are flavonoids present in hypericum that are claimed to be responsible for the antidepressant activity of the plant. The contributing mechanisms of action include inhibition of the reuptake of serotonin (5-HT), dopamine (DA), norepinephrine (NE) in the. synaptic cleft, binding to the GABA-A and GABA-B receptors thereby inhibiting the binding of GABA ligands, increasing the density of 5-HT2 receptors in the frontal cortex of the brain. Other medicinal plants most widely used to treatment depression around the world are Centella asiatica, Rhodiola rosea, Pfaffia paniculata, Rauwolfia serpentina, Rhododendron molle, Schizandra chin, Thea sinensis, Uncaria tome, Valeriana officinalis and Withania somnifera. Plants such as Justicia odora, Calpurnia aurea and Asparagus leptocladodius have traditionally been used for the treatment of depression. [11], [12]
Comparative Features of Therapeutic Groups
In general, between 50 and 70% of patients respond to the first antidepressant, irrespective of its pharmacological profile. [Table 3]
|
|
Tricyclic antidepressants |
SSRIs |
SNRIs |
|
Efficiency rate |
About 70% |
About 70% |
About 70% |
|
Onset of action |
Takes 3-6 weeks to work (although some people respond earlier) |
Takes 3-6 weeks to work (although some people respond earlier) |
Takes 3-6 weeks to work (although some people respond earlier) |
|
Anticholinergic action |
Strong |
Lesser than TCA |
Lesser than TCA |
|
Adverse effects on digestive system ie nausea |
Minimal |
More |
Less |
|
Interaction with other drugs |
Almost insignificant |
Significant in some cases |
Not significant |
|
Effect on disease other than depression |
Panic disorder and obsessive compulsive disorder |
Panic disorder and obsessive compulsive disorder |
Efficacy on some anxiety disorders is documented |
Selective serotonin reuptake inhibitors (SSRI), Serotonin-noradrenaline reuptake inhibitor (SNRI) [13]
Recommended Guidelines for pharmacotherapy
Major Depressive Disorder
There are multiple therapeutic approaches to treating depression. These plans include the Texas Medication Algorithm Project (TMAP), the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trials, and the American Psychiatric Association (APA) Treatment Guidelines.
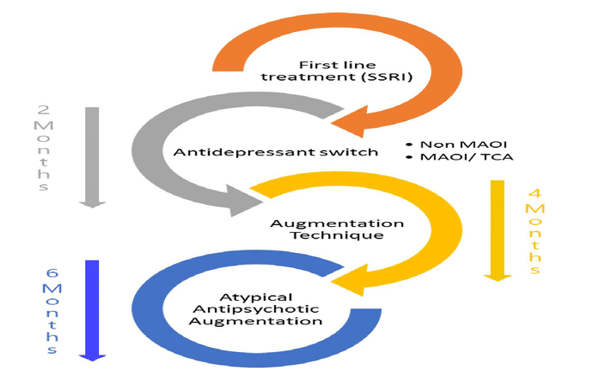
30% of depressed persons seek medical treatment, and of those treated, about 30% effectively achieve remission. Medications used to treat depression include SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), MAOIs, tricyclic antidepressants (TCAs), central alpha2-receptor antagonists, and norepinephrine and dopamine reuptake inhibitors.[14] [[Figure 3] ]
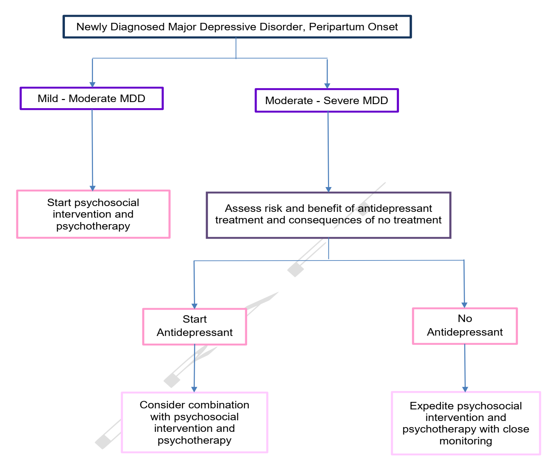
Treatment Algorithm of Major Depressive Disorder (BC Guidelines on Depression 2017) [Figure 4] [14], [15]

Post partum depression
Top choice among these is sertraline, the most widely studied antidepressant in breast-feeding mothers and their infants. While small amounts enter breast milk, little or no medication can be detected in infants, and there appear to be no adverse effects. Paroxetine is also a highly-rated choice. Paroxetine is not detectable in breast milk or nursing infants. Two other widely used SSRIs, fluoxetine and citalopram , enter breast milk in small amounts but are viewed as acceptable alternatives. [15], [16]
Bipolar Disorder
Lithium is mainly used to treat bipolar disorder, which is characterized by recurrent episodes of depression, mania, and hypomania. However, lithium is also used as an adjunctive medication in patients who have inadequately responded to an antidepressant for treatment of unipolar depression (ie, depression with no lifetime history of mania or hypomania)
The following algorithm is followed[17] [[Figure 4]]

Atypical Depression
In most cases, treatment includes a combination of medications, talk therapy, and lifestyle changes. Patients with atypical depression have been shown to have less or no response to TCAs and better response to MAOIs. Fluoxetine was equally effective to phenelzine, an MAOI, in atypical depression. MAOIs with SSRI are also used. [18]
Seasonal Affective Disorder
Cognitive behavioural therapy (CBT) - form of psychotherapy is helpful. Light therapy is one of the first line treatments for fall-onset SAD. It generally starts working in a few days to a few weeks and causes few side effects. Selective serotonin reuptake inhibitors (SSRIs) are the preferred type of antidepressant for treating SAD [19]
Pyschotic Depression
The combination of an antidepressant plus an antipsychotic provides more effective treatment for psychotic depression than either treatment alone, as evidenced by Cochrane Analysis [20]
Persistent depressive disorder (Dysthymia)
Antidepressants, especially noradrenergic agents, are useful for depression-related apathy. However, selective serotonin reuptake inhibitors (SSRIs) may be less effective for apathy in depressed elderly patients and have even been reported to worsen apathy. Dopaminergic agonists seem to be effective for apathy. Acetylcholine esterase inhibitors, methylphenidate, atypical antipsychotics, nicergoline, and cilostazol are another choice. Medication choice should be determined according to the background and underlying etiology of the targeting disease [21]
Depression Algorithm in Elderly[22]:
Citalopram, moclobemide, and probably fluoxetine are more effective than placebo in older depressed patients. The serotonin reuptake inhibitors fluvoxamine, paroxetine, and sertraline as well as milnacipran and venlafaxine are probably (but not unequivocally) as effective as older antidepressants
Monitoring Serum Levels of antidepressants
Therapeutic Drug Monitoring
Can be of help in situations in which patients are refractory to therapy despite adequate or high dosages, when adverse events supervene even with low doses, or when noncompliance with the intended dosage plan is suspected. the clinical use of monitoring plasma concentrations of the TCAs imipramine, desipramine, and nortriptyline. Therapeutic monitoring of amitriptyline is also accepted, based in part on its metabolism to nortriptyline. Additionally, evidence for plasma concentration vs response relationships for doxepin , clomipramine , and bupropion has been reported. Therapeutic ranges for the antidepressants maprotiline, amoxapine, trazodone, and alprazolam have also been suggested However, no general consensus has been achieved. [23]
Dose of antidepressants used: [[Table 5] ] [24]
|
Line |
Medication [2] |
Initial dose |
Titration schedule if unsatisfactory clinical response after 2-4 week, then: |
Usual therapeutic dose range |
|
1st |
Escitalopram |
Mg daily × 7 days, then increase to 10 mg daily. |
Increase to 20 mg daily. |
10-20 mg |
|
|
Fluoxetine |
10 mg daily before noon × 7 days, then increase to 20 mg daily before noon. |
Increase by 20mg increments at 4-week intervals. |
20-60 mg |
|
|
Sertraline |
50 mg daily × 7 days, then increase to 100 mg daily |
Increase in 50 mg increments at 4-week intervals. |
50-200 mg |
|
2nd |
Bupropion SR |
150 daily in the morning × 7 days, then increase to 150 mg b.i.d |
Increase to 200 mg b.i.d |
300-400 mg |
|
|
Bupropion SR |
150 mg daily in the morning |
Increase to 200 mg b.i.d |
300-450 mg |
|
|
Citalopram [3] |
10 mg daily × 7 days, the increase to 20 mg daily. |
Increase to 40 mg unless patient is over 60 years of age |
20-40 mg |
|
|
Mirtazapine |
15 mg daily at bedtime × 7 days, then increase to 30mg daily at bedtime. |
Increase to 45 mg daily bedtime. |
15-45 mg |
|
|
Paroxetine |
10 mg daily × 7 days, then increase to 20 mg daily |
Increase by 10 mg increment at 4-week intervals. |
10-50 mg |
|
|
Venlafaxine XR (caps preferred) |
75 mg daily with food × 7 days, the increase to 150 mg daily |
Increase to 225 mg daily. |
75-225 mg. |
Side Effects
Patients must take the antidepressant for 3–4 weeks before they are likely to experience a therapeutic effect. Stopping it suddenly may lead to withdrawal symptoms such as anxiety and irritability, or depression may recur. Many people have at least one side effect.
The relationship between antidepressants, especially serotonin reuptake inhibitors, and suicidal ideation and behavior has received considerable public attention lately. The use of these drugs in children and adolescents has been of particular concern. Common side effects of serotonin reuptake inhibitors in the elderly are nausea, insomnia, and sedation.
Tricyclic antidepressants should be started with very low doses. Alpha-1 adrenergic blockade leads to orthostatic hypotension, which can cause dizziness and falls in the elderly. Histaminic effects can cause sedation and weight gain.
Trazodone can cause significant orthostatic hypotension, dizziness, and headache. In rare cases, it can cause priapism.
Serotonin discontinuation syndrome has been described in children. Serotonin discontinuation syndrome is a condition in which the patient experiences unpleasant physical withdrawal symptoms if the SSRI is stopped abruptly. Symptoms include dizziness, nausea, vomiting, tiredness, headache, gait and sleep disturbance. These are reported to occur within 1–3 days after stopping the SSRI in those antidepressants with a short half-life [25].
Drug interactions with monoamine oxidase inhibitors
If the patient is taking MAOIs, certain aged, fermented, or pickled foods must be avoided, like many wines, processed meats, and cheeses. MAOI can cause dangerously high levels of serotonin, known as serotonin syndrome. It most often occurs when two medications that raise serotonin are combined. These include, for example, other antidepressants, certain pain or headache medications, and the herbal supplement St. John's wort. MAOI also interact with many drugs.
|
Class |
Examples |
|
SSRIs |
Fluoxetine, Paroxetine, Sertraline |
|
SNRIs |
Duloxetine, Venlafaxine |
|
TCA |
Imipramine, Amityptyline |
|
Tetracyclic antidepressant |
Mirtazapine |
|
Other |
Buspirone, Bupropion |
|
Analgesics |
Meperidine, Methadone , Tramadone, Propoxyphene |
|
Cold preparations |
Dextromethorphan, ephedrine, phenylephrine, pseudoephedrine |
Somatic Therapy
A device-based approach that consists of introducing transient electric or magnetic current onto the scalp or to anatomically deep brain structures. The mechanism of action is largely attributed to increasing the level of neurotransmitters and sensitization of post synaptic receptors through changing the neuronal firing in the regions involved. Electroconvulsive therapy (ECT) is the first effective somatic therapy to be used for the treatment of mental disorders with a widespread clinical use even up to now. Transcranial magnetic stimulation (TMS) is another type of somatic treatment option for treatment resistant depression. TMS induces depolarization of cortical neurons by the use of magnetic current that passes through a metal coil applied to the scalp of the patient. Vagus nerve stimulation (VNS) is a minimally invasive procedure where an impulse generator device is implanted in the chest area of the patient attached to the left vagus nerve with lead wires. [25], [26]
Conclusion
Studies show that the benefit generally depends on the severity of the depression. The more severe the depression, the greater the benefits will be. In other words, antidepressants are effective against chronic, moderate and severe depression. The commonly used tricyclic antidepressants (SSRIs and SNRIs) were found to be equally effective. Antidepressant may lose its effect after months or years, sometimes because the brain has become less responsive to the drug (tolerance). Solutions include increasing the dose and switching to another antidepressant with a different mechanism of action. The lifetime suicide rate of people with major depression is 15%, and depression can also be lethal in other ways; for example, a history of major depression doubles the risk of heart disease. The majority of depressed patients should be treated with a low dosage of SSRIs and SNRI, generally corresponding to one tablet per day.
Source of Funding
None.
Conflict of Interest
None.
References
- Entzeroth M, Ratty AK. Monoamine Oxidase Inhibitors—Revisiting a Therapeutic Principle. Open J Depress. 2017;06(02):31-68. [Google Scholar]
- . American Psychiatric Association. . . [Google Scholar]
- Hanwella R, Silva VD. Diagnosis and management of depression. Ceylon Med J. 2008;53(2):60-2. [Google Scholar]
- Grover S, Dutt A. Ajit Avasthi, An overview of Indian research in depression. Indian J Psychiatry. 2010;52. [Google Scholar]
- Saveanu RV, Nemeroff CB. Etiology of Depression: Genetic and Environmental Factors. Psychiatric Clin North Am. 2012;35(1):51-71. [Google Scholar]
- Yang L. The Effects of Psychological Stress on Depression. Curr Neuropharmacol. 2015;13:494-504. [Google Scholar]
- . https://www.psycom.net/depression.central.html. . . [Google Scholar]
- . https://www.webmd.com/depression/guide/depression-types#3-6. . . [Google Scholar]
- Thomas E. The diagnosis and management of depression in the era of the DSM-5 South African Family Practice. . 2018;60:22-8. [Google Scholar]
- Hatcher S. Newer antidepressants. BMJ. 2012;344. [Google Scholar]
- Khushboo, Sharma B. Factors inducing depression as effective tool in therapy. Med Clin Arch. 2019;3(4). [Google Scholar]
- Fekadu N. Major Depressive Disorder: Pathophysiology and Clinical Management. J Depress Anxiety. 2017;6. [Google Scholar]
- Soichiro N. Characteristics and Use of New Antidepressant Drugs. JMAJ. 2004;47(6):265-9. [Google Scholar]
- Madhukar H, Trivedi. Use of Treatment Algorithms for Depression. Prim Care Companion J Clin Psychiatry. 2006;8(5):291-8. [Google Scholar]
- Clinical, Guidelines, Management Of Major, Depressive Disorder. . Ministry of Health. . [Google Scholar]
- . . . . [Google Scholar]
- Shah N, Grover S, Rao G. Clinical Practice Guidelines for Management of Bipolar Disorder. Indian J Psychiatr. 2017;59(5). [Google Scholar]
- Singh T. Atypical Depression . Psychiatry (Edgmont). 2006;3(4):33-9. [Google Scholar]
- . SAD, Mayo Clinic Proceedings . . 2019. [Google Scholar]
- Cochrane. Pharmacological treatment for psychotic depression Version published. . 2015. [Google Scholar]
- Ishizaki J, Mimura M. Dysthymia and Apathy: Diagnosis and Treatment Depression Research and Treatment. . 2011. [Google Scholar]
- Reuben DB, Herr KA, Pacala JT, Pollock BG. Geriatrics at Your Fingertips. 2014. 16th edition. And American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. . 2013. [Google Scholar]
- Mark W, Linder. Standards of laboratory practice: antidepressant drug monitoring. Clinical Chemistry. 1998;44(5):1073-1084. [Google Scholar]
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview.. Cleveland Clin J Med. 2006;73(4):351-3. [Google Scholar]
- Fekadu N, Shibeshi W, Engidawork E. Major Depressive Disorder: Pathophysiology and Clinical Management.. J Depress Anxiety. 2017;06(01). [Google Scholar]
- Hegarty K. Antidepressants in GP Setting. Australian Family Physician. 2003;32(4). [Google Scholar]
- Abstract
- Introduction
- Definition
- Causes of Depression
- Immunological
- Biochemical
- Drug and alcohol abuse
- Medical conditions
- Trauma
- Cancer
- Life circumstances
- Post partum depression
- Types of Depression
- Diagnosing Depression
- Mechanism of Antidepressants
- Herbal Drugs
- Comparative Features of Therapeutic Groups
- Recommended Guidelines for pharmacotherapy
- Bipolar Disorder
- Atypical Depression
- Seasonal Affective Disorder
- Pyschotic Depression
- Persistent depressive disorder (Dysthymia)
- Depression Algorithm in Elderly[22]:
- Monitoring Serum Levels of antidepressants
- Dose of antidepressants used: [[Table 5] ] [24]
- Side Effects
- Drug interactions with monoamine oxidase inhibitors
- Somatic Therapy
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Chaudhry S. Depression and its Dilemma [Internet]. IP J Surg Allied Sci. 2020 [cited 2025 Nov 02];2(3):81-88. Available from: https://doi.org/10.18231/j.jsas.2020.013
APA
Chaudhry, S. (2020). Depression and its Dilemma. IP J Surg Allied Sci, 2(3), 81-88. https://doi.org/10.18231/j.jsas.2020.013
MLA
Chaudhry, Sunil. "Depression and its Dilemma." IP J Surg Allied Sci, vol. 2, no. 3, 2020, pp. 81-88. https://doi.org/10.18231/j.jsas.2020.013
Chicago
Chaudhry, S.. "Depression and its Dilemma." IP J Surg Allied Sci 2, no. 3 (2020): 81-88. https://doi.org/10.18231/j.jsas.2020.013
