- Visibility 63 Views
- Downloads 12 Downloads
- Permissions
- DOI 10.18231/j.jsas.2020.017
-
CrossMark
- Citation
Mitigating Psychosis
- Author Details:
-
Sunil Chaudhry *
Abstract
Young males are more likely to experience first-episode psychosis, compared to women in the same age group. Prevalence of schizophrenia is 2.5/1000 and which seems to be the only disorder whose prevalence is consistent across cultures and over time. Genetic factors play an important role in the causation of schizophrenia; the risk of illness is approximately 10% for a first-degree relative and 3% for a second-degree relative. According to the American Psychiatric Association, second-generation (atypical) antipsychotics with the exception of clozapine are the agents of choice for first-line treatment of schizophrenia. Clozapine is not recommended because of its risk of agranulocytosis. A combination of antipsychotic showed an improvement in symptoms, but the side effects need to be monitored.
Introduction
Defining psychosis
Psychosis is used to describe conditions that affect the mind, where there has been some loss of contact with reality. Symptoms of psychosis include delusions (false beliefs) and hallucinations (seeing or hearing things that others do not see or hear). Other symptoms include incoherent or nonsense speech, and behaviour that is inappropriate for the situation.[1]
Types of psychosis
Schizophrenia spectrum” (DSM-5 terminology) or the group of “schizophrenia and other primary psychotic disorders are classified
Brief psychotic disorder : There are three different possible types of brief psychotic disorder:
Brief psychotic disorder with a marked stressor(s) - When a psychotic episode is triggered by an emotionally stressful event or events in an individual’s life
Brief psychotic disorder without a marked stressor(s) – When a psychotic episode occurs without any stressful event acting as a trigger
Brief psychotic disorder with postpartum onset – When a psychotic episode occurs during pregnancy or within the 4 weeks postpartum.
Common symptoms are Delusions, hallucinations, disorganised speech, catatonic behaviour.[2]
Drug- or alcohol-related psychosis: Drugs, including stimulants such as methamphetamine and cocaine. Drugs like steroids and stimulants can also cause symptoms of psychosis. Psychosis associated with alcohol can occur with acute intoxication, alcohol withdrawal, as well as in chronic alcoholics
Organic psychosis: An organic psychosis is an organic (ie physical) disease, which causes mental illness. It can either be a disease of the brain (eg embolism, infection, tumour or trauma)
Schizoaffective disorder: People have symptoms of both schizophrenia and a mood disorder, such as depression or bipolar disorder.
Schizophreniform disorder: This includes symptoms of schizophrenia but the symptoms last for a shorter time: between 1 and 6 months.
Schizophrenia: DSM (Diagnostic and Statistical Manual of Mental Disorders) -5 have following as listed criteria:
Two or more of the following for at least a one-month (or longer) period of time, and at least one of them must be 1, 2, or 3:
Delusions
Hallucinations
Disorganized speech
Grossly disorganized or catatonic behaviour
Negative symptoms, such as diminished emotional expression
Schizophrenia: is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking.
Paranoid-type schizophrenia is distinguished by paranoid behaviour, including delusions and auditory hallucinations. Paranoid behaviour is exhibited by feelings of persecution, of being watched,
A person with disorganized-type schizophrenia will exhibit behaviours that are disorganized or speech that may be bizarre or difficult to understand.
Catatonic Schizophrenia: People with this type of schizophrenia may vary between extremes: they may remain immobile or may move all over the place.
Undifferentiated-type schizophrenia is a classification used when a person exhibits behaviours which fit into two or more of the other types of schizophrenia.
Residual Schizophrenia: When a person has a past history of at least one episode of schizophrenia, but the currently has no symptoms.[3], [4]
Symptoms: Psychotic symptoms can generally be divided into positive, negative, and cognitive symptoms. [[Table 1]]
Cognitive Impairment: These impairments include problems with attention, memory, and executive function (i.e., abstraction, problem-solving, insight, and cognitive flexibility).
|
Positive Symptoms |
Negative Symptoms |
|
Hallucinations |
Affective flattening |
|
Delusions |
Alogia / Avolition / Anhedonia |
|
Disorganised behaviour |
Asocial |
|
Disturbed language |
|
Mood symptoms are commonly present in individuals with psychotic symptoms and usually require treatment.[5]
|
Sleep disturbance (increased or decreased) |
Morbid preoccupation or suicidal ideation |
|
Appetite disturbance (increased or decreased) |
Decrease or increase in goal directed activities |
|
Disturbances in energy level (agitation, hyperactivity, or low energy) |
Disturbances in self image (low self esteem or grandiosity) |
|
Poor concentration or distractibility |
Disturbances in mood (depressed, euphoric, irritable or mixed) |
|
Excessive guilt or shame |
Change in rate of thought processing (increased or decreased) |
|
Thoughts of harm toward others |
Change in quantity and rate of speech (increased or decreased) |
The cognitive symptoms are the most disabling and misunderstood of all the symptom complexes associated with psychotic disorders.[6]
Cause of psychosis
Psychosis may occur as a result of many conditions. Psychosis is most commonly found in mental illnesses, including psychotic disorders and mood disorders. Psychosis can be related to many other things, including: The use of cannabis (marijuana). Cannabis has been linked to the onset of schizophrenia in some studies Other causes of psychosis include alcohol and other illegal drugs such as amphetamine (speed), cocaine, methamphetamine, mephedrone MDMA (ecstasy), LSD (acid), psilocybin (mushrooms), ketamine and opiates (heroin). Physical issues such as epilepsy, Parkinson’s disease, Wilson’s disease (inability to process copper), Huntington’s disease, chromosomal disorders, brain tumours, dementia, Lyme disease, multiple sclerosis and stroke. Lack of sleep, Very poor nutrition. The use of some prescription drugs, such as steroids, opiates (codeine, morphine) and stimulants, including medication for ADHD (Attention deficit hyperactivity disorder).[7]
Mechanisms of Psychosis
Biochemical
Glutamate is the most abundant excitatory neurotransmitter in the cerebral cortex. Although the common antipsychotics act on dopamine receptors, the hypofunction of the ionotropic glutamate N-methyl-D-Aspartate (NMDA) receptor has been proposed as a mechanism in schizophrenia.8]
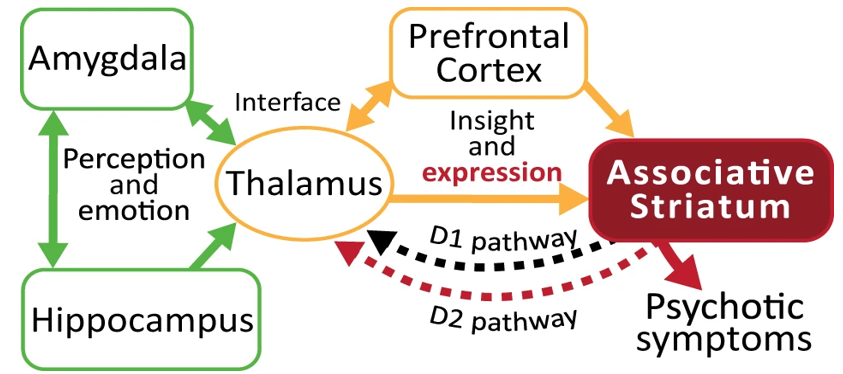
In the case of schizophrenia, the dopamine hypothesis proposes that dopamine transmission is overactive in the mesolimbic areas and underactive in the prefrontal cortex. Dopamine dysregulation is also seen in the amygdala, which is involved in emotional processing. The positive symptoms of schizophrenia are hyperactive dopaminergic signal transduction. The overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder. [Figure 1][8]
The Role of Serotonin in Schizophrenia: Decreased levels of 5-hydroxyindoleacetic acid in cerebrospinal fluid have been found to be correlated with cortical atrophy or ventricular enlargement in schizophrenic patients. There is increasing interest in the correlation between negative symptoms of schizophrenia and 5-HT(2) receptors. The rationale for these studies is the hypothesis that abnormal neurotransmission at 5-HT(2) receptors may be involved in the pathophysiology of schizophrenia. [9]
Cytokines: Increased levels of IL-6 in different groups of patients including, first-episode and drug-naive (FEDN) psychosis patients. Multiple studies, including meta-analyses, reported elevated levels of TNF-α, one of the other pro-inflammatory cytokines. Several studies, including some meta-analyses, found elevated levels of IFN-γ in chronic schizophrenic patients who were stable or were experiencing an acute relapse.
Glycine is an α-amino acid, which also has a role as an inhibitory neurotransmitter via binding to strychnine-sensitive glycine receptors. Some randomized controlled trials (RCT) with oral glycine suggested improvement of negative symptoms. D-serine or D-alanine also have shown efficacy for the treatment of negative symptoms.[10]
Epigenetic mechanisms encompass several pathways that can mediate gene-by-environment interactions and modulate gene expression and activity without altering the DNA sequence. These include, among others, DNA methylation, histone modifications, chromatin remodeling, and the actions of noncoding RNAs. [11]
Principles of antipsychotic prescribing
Treatment with antipsychotic medication, like any other treatment, should be individualized in order to optimally promote recovery.
Treatment with antipsychotic medication should be as effective, safe, and well tolerated as possible
Treatment with antipsychotic medication should consider personal preference and vulnerabilities.
Treatment with antipsychotic medication should provide value in terms of improved quality of life to the consumer.
Treatment choices should be informed by the best current evidence and must evolve in response to new information.
Cost considerations should guide antipsychotic medication selection once the preceding principles are met.[12]
Classification of antipsychotic drugs: Table 3: [ESPE -extrapyramidal side effects]
|
Antipsychotic All antipsychotics can cause hyperlactinaemia |
Characteristic |
|
Conventional antipsychotics |
|
|
Chlorpromazine, Pericyazine |
Most sedating, most potent anticholinergic effects, least likely to cause EPSE, most likely to cause orthostatic hypotension; sometimes referred to as low potency antipsychotics. |
|
Trifluoperazine, Fluphenazine |
Moderately sedating; intermediate propensity to cause EPSE, some potential to cause orthostatic hypotension. |
|
Haloperidol, Droperidol, Thiothixene, Pimozide |
Least sedating, almost no anticholinergic effects, most likely to cause EPSE, least likely to cause orthostatic hypotension; sometimes referred to as high potency antipsychotics. |
|
Atypical antipsychotics |
|
|
Atypical agents have less potential for EPSE than conventional agents, but depends on dose |
|
|
Amisulpride |
Less potential for weight gain and sedation |
|
Aripiprazole |
May cause insomnia, less potential for hyperprolactinaemia |
|
Clozapine |
Effective in treatment-resistant patients but has serious adverse effects (blood dyscrasias, seizures, cardiomyopathy, myocarditis, orthostatic hypotension, sedation, weight gain) |
|
Olanzapine |
Related to clozapine may cause sedation, weight gain, peripheral oedema; increased risk of stroke and related mortality in elderly dementia patients. |
|
Quetiapine |
Sedating and vasoactive less potential for hyperprolactinemia. |
|
Risperidone, Paliperidone |
Orthostatic and vasoactive less potential for hyperprolactinemia. |
|
Ziprasidone |
Less potential for weight gain. |
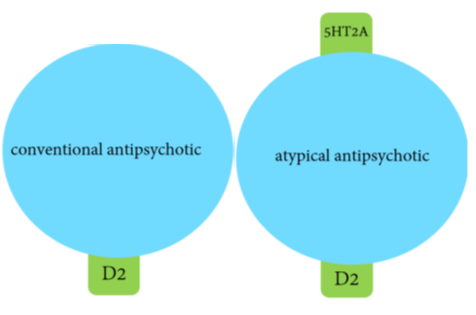
Typical Antipsychotic drugs such as haloperidol , Thiothixene chlorpromazine also referred as FGA (First generation antipsychotics) tend to block dopamine D2 receptors in the dopaminergic pathways of the brain. Excess release of dopamine in the mesolimbic pathway has been linked to psychotic episodes.
Atypical antipsychotic drugs or second generation antipsychotics (SGA) have a similar blocking effect on D2 receptors; however, most also act on serotonin receptors, especially 5-HT2A and 5-HT2C receptors. Both clozapine and quetiapine appear to bind just long enough to elicit antipsychotic effects but not long enough to induce extrapyramidal side effects and prolactin hypersecretion.[13]
Therapeutic drug monitoring
Therapeutic drug monitoring is not strictly necessary for all of the new antipsychotic drugs because there are no unequivocal data supporting a relationship between plasma drug levels and clinical outcomes or side effects. There has been success in defining the minimum therapeutic response threshold for certain antipsychotics—for example, clozapine (350 to 450 ng/mL), haloperidol (3 to 5 ng/mL), and fluphenazine (0.8 ng/mL).[14], [15]
Guidance on the use of Antipsychotics
The antipsychotic medications have two applications:
Reduce severe or acute symptoms to a level, where they are manageable. Sometimes the effect is seen early but in general it takes 2-4 weeks to show response
Prevention of relapses.
With the exception of clozapine, the efficacy of all antipsychotics is very similar andoften the choice is governed by the side effect profile of the antipsychotic. Poor compliance with oral antipsychotics is common in patients with schizophrenia, mania and other psychoses which often results in a relapse of the illness. The use of depot medication can be considered for use in these situations as it promotes adherence to medication, allows for earlier detection of non-adherence with the potential for earlier intervention and possible decreased risk of severe relapse. All patients receiving long term treatment with antipsychotic medication should be monitored routinely and regularly. Treatment resistance is described as being resistant to adequate trials of at least two antipsychotics. In such circumstances service users must be offered a trial of clozapine at the earliest opportunity. Clozapine started given with monitoring of white blood cells (WBCs) count. By its heavy dose if agranulocytosis occurs then must discontinue the clozapine. Augmentation therapy is given with second generation antipsychotics combine with electroconvulsive therapy (ECT) Currently, effective treatments for cognitive deficits are thought to be the greatest unmet needs. Numerous recent clinical trials have suggested only modest benefits on cognitive function in schizophrenia relative to first- and second-generation antipsychotics when dosed properly.[16], [17]
Switching from one antipsychotic to another is frequently indicated due to an inadequate treatment response or unacceptable adverse effects. It should be carried out cautiously and under close observation. There are a number of clinical situations in which switching from one antipsychotic to another is considered.
Inadequate clinical response for acute symptoms despite dose optimisation and adequate duration of treatment trial.
Poor control of chronic symptoms and persistence of functional disabilities during maintenance therapy.
Relapse despite adequate prophylactic or maintenance treatment of a psychotic illness.
Persistence of certain symptoms of psychotic illness (e.g. negative symptoms and cognitive dysfunction) despite adequate doses of one antipsychotic, which may respond better to an alternative drug.
Unacceptable adverse effects at low therapeutic doses before a clinical response in susceptible individuals (e.g. extrapyramidal effects in Asian patients). Consider switching to an antipsychotic with a lower risk for the adverse effect.[18]
Algorithm- Antipsychotic Selection in Schizophrenia and Schizoaffective Disorder [[Figure 2]]
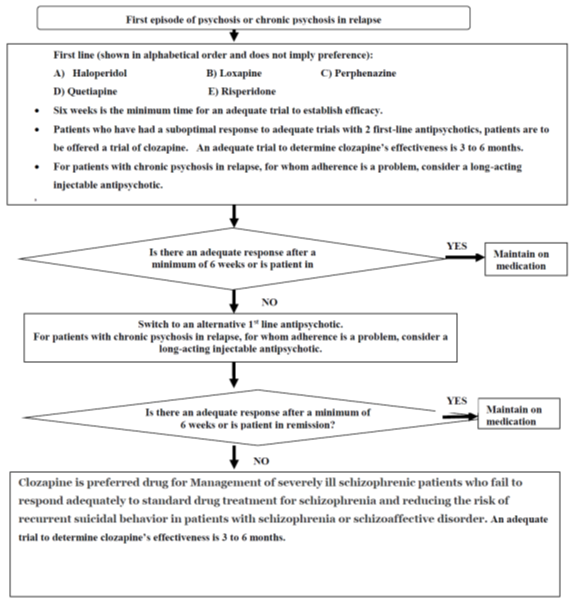
Primary indications for Clozapine is in patients with schizophrenia or schizoaffective disorder are schizophrenia symptoms partially or fully resistant to treatment with other antipsychotic drugs, or accompanied by persistent suicidal or self-injurious behaviour.[19], [20], [21]
Glycine therapy
Glycine (an amino acid sold as a dietary supplement) has been a subject of research for over 15 years as a potential treatment for the negative symptoms of schizophrenia. Clinical trials suggest that the optimal dosage may be in the range of 30 grams to 60 grams a day. The biggest downside to taking glycine seems to be upset stomach and nausea. Glycine may turn out to be a beneficial supplemental treatment (when added to standard antipsychotic medications).[22]
ADR Profile of antipsychotics
The effects range from relatively minor tolerability issues (e.g., mild sedation or dry mouth) to very unpleasant (e.g., constipation, akathisia, sexual dysfunction) to painful (e.g., acute dystonia) to disfiguring (e.g., weight gain, tardive dyskinesia) to life-threatening (e.g., myocarditis, agranulocytosis). Parkinsonism, tardive dyskinesia, neuroleptic malignant syndrome and hyperprolactinemia are considered to be a result of acute or chronic blockade of DA receptors, while histamine-H1 and 5-HT2Creceptors may contribute to antipsychotic-induced weight gain.
Neuroleptic malignant syndrome (NMS) is a life-threatening emergency that closely resembles malignant hyperthermia (MH). It is characterized by hyperthermia, muscle rigidity, severe hypermetabolic dysautonomia, and mental status changes. It can be triggered by a single dose of any antipsychotic, but is most commonly associated with the high potency FGAs, including haloperidol and droperidol. MH, first-line management is dantrolene (0.5-2.5 mg/kg every 6-12 hours), aggressive hydration, and supportive management.
Adverse events of antipsychotics reduce patients' quality of life, compliance with taking the antipsychotics (and thereby also relapse) and the stigma experienced. Other features can include neutrophilia and occasionally haemorrhagic tendency [23], [24], [25]
The American Psychiatric Association's latest guidance recommends thorough physical exam and laboratory screening, with ECG.
|
|
High |
Mid |
Low |
|
Conventional antipsychotics |
Thioridazine |
Chlorpromazine |
Haloperidol |
|
Atypical Antipsychotics |
Ziprasidone |
Quetiapine |
Risperidone |
|
|
|
|
Clozapaine |
|
|
|
|
Olanzapine |
|
|
|
|
Aripiprazole |
Antipsychotics are associated with a 1.5 to 4‐fold increase in risk of sudden cardiac death. There is no evidence that second‐generation antipsychotics are safer than first‐generation drugs as a class.
Natural Medicines for Psychosis
In 110 randomized controlled trials, evidence was found for glycine, sarcosine, N-acetylcysteine, some Chinese and ayurvedic herbs, ginkgo biloba, and estradiol to improve psychotic symptoms when added to antipsychotics. Ginkgo biloba and vitamin B6 seemed to reduce tardive dyskinesia and akathisia. Inconsistent beneficial outcomes of studies on B vitamins were, especially when given as a combination of B1, B3, B9, and/or B12 with antipsychotics. No adequate support for the efficacy of B vitamins in schizophrenia can be identified, except B6 [26]
Conclusion
Antipsychotic medications are the mainstay t for psychosis, with second-generation antipsychotic (SGA) medications generally considered the drugs of first choice Conventional and atypical antipsychotics are used as the foundation for the pharmacological management of schizophrenia and related psychosis. All antipsychotics are considered to be of equal efficacy, with the exception of Clozapine. The newer atypical agents are generally better tolerated and have less EPSE than the older conventional agents. It has long been recognized that conventional antipsychotics can increase the risk of EPS and tardive dyskinesia in elderly patients, so atypical antipsychotic has gradually replaced conventional antipsychotics in elderly patients. Notwithstanding controversial data, antipsychotics are probably the best option for short-term treatment (6–12 weeks) of severe, persistent, and resistant aggression. The possibility of serious adverse events restricts long-term therapy and clinician should decrease dosage and discontinue treatment wherever a sufficient control of behavioural symptoms has been obtained.
Conflict of Interest
None declared
Source of Funding
None.
References
- . National Institute of mental health . . . [Google Scholar]
- . Diagnostic and Statistical Manual of Mental Disorders. 5th Edn.. 2013. [Google Scholar]
- . https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms. . . [Google Scholar]
- Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S. Jim Van Os , William Carpenter Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;1(3):3-10. [Google Scholar]
- Andreasen N, Flaum M, II VWS, Tyrrell G, Arndt S. Positive and Negative Symptoms in Schizophrenia. Arch General Psychiatry. 1990;47(7):615-21. [Google Scholar] [Crossref]
- Tripathi A, Kar S, Shukla R. Cognitive Deficits in Schizophrenia: Understanding the Biological Correlates and Remediation Strategies. Clin Psychopharmacol Neurosci. 2018;16(1):7-17. [Google Scholar] [Crossref]
- . Understanding psychosis, Resources and recovery , National alliance on mental illness. . . [Google Scholar]
- Tost H, Alam T, Meyer-Lindenberg A. Dopamine and psychosis: Theory, pathomechanisms and intermediate phenotypes. Neuroscie Biobehavioral Rev. 2010;34(5):689-700. [Google Scholar] [Crossref]
- Kesby J, Eyles D, McGrath J, Scott J. Dopamine, psychosis and schizophrenia: the widening gap between basic and clinical neuroscience. Transl Psychiatry. 2018;8(1). [Google Scholar] [Crossref]
- Kalus O, Asnis GM, Praag HMv. The Role of Serotonin in Depression. Psychiatric Ann. 1989;19(7):348-53. [Google Scholar] [Crossref]
- Momtazmanesh S, Zare-Shahabadi A, Rezaei N. Cytokine Alterations in Schizophrenia: An Updated Review. Front Psychiatry. 2019;10. [Google Scholar]
- Smigielski L, Jagannath V, Rössler W, Walitza S, Grünblatt E. Epigenetic mechanisms in schizophrenia and other psychotic disorders: a systematic review of empirical human findings. Mol Psychiatry. 2020;25(8):1718-48. [Google Scholar] [Crossref]
- Kaur H, Maurya P, Kaur R. Antipsychotic Drugs. Advances in Neuropharmacology. . [Google Scholar]
- Laruelle M. Mechanism of action of antipsychotic drugs. Clin Ther. 2005;27:16-24. [Google Scholar]
- Cooper T. Plasma Level Monitoring of Antipsychotic Drugs. Clin Pharmacokinetics. 1978;3(1):14-38. [Google Scholar] [Crossref]
- Jonathan M. Meyer, is monitoring of plasma antipsychotic levels useful?, . Curr Psychiatry. 2015;14(11):19-20. [Google Scholar]
- . NHS trust, Guidance on the use of antipsychotics. . 2018. [Google Scholar]
- Victor I, Reus. The American Psychiatric Association Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients With Dementia. . 2012. [Google Scholar]
- Keks N, Schwartz D, Hope J. Stopping and switching antipsychotic drugs. Aust Prescr. 2019;42(5):152-7. [Google Scholar] [Crossref]
- . VA Pharmacy Benefits and Advisory Panel , Selection in schizophrenia and schizoaffective disorder. . 2012. [Google Scholar]
- . Selection of antipsychotics. . 2019. [Google Scholar]
- . http://schizophrenia.com/treatments.php#. . . [Google Scholar]
- Zeeshan ZM. Schizophrenia: An overview. Clin Pract. 2018;15(5):847-51. [Google Scholar]
- Pryor K, Storer KP. Pharmacology and Physiology for Anesthesia. . 2013. [Google Scholar]
- Ucok A. Side effects of atypical antipsychotics: A brief overview. J World Psychiatric Assoc (WPA). 2008;7(1):58-62. [Google Scholar]
- Hoenders HR, Bartels-Velthuis A, Vollbehr N, Bruggeman R, Knegtering H, Jong Jd. Natural Medicines for Psychotic Disorders. J Nerv Mental Dis. 2018;206(2):81-101. [Google Scholar] [Crossref]
- Abstract
- Introduction
- Mechanisms of Psychosis
- Biochemical
- Principles of antipsychotic prescribing
- Therapeutic drug monitoring
- Guidance on the use of Antipsychotics
- Glycine therapy
- ADR Profile of antipsychotics
- Natural Medicines for Psychosis
- Conclusion
- Conflict of Interest
- Source of Funding
- References
How to Cite This Article
Vancouver
Chaudhry S. Mitigating Psychosis [Internet]. IP J Surg Allied Sci. 2020 [cited 2025 Sep 14];2(4):102-107. Available from: https://doi.org/10.18231/j.jsas.2020.017
APA
Chaudhry, S. (2020). Mitigating Psychosis. IP J Surg Allied Sci, 2(4), 102-107. https://doi.org/10.18231/j.jsas.2020.017
MLA
Chaudhry, Sunil. "Mitigating Psychosis." IP J Surg Allied Sci, vol. 2, no. 4, 2020, pp. 102-107. https://doi.org/10.18231/j.jsas.2020.017
Chicago
Chaudhry, S.. "Mitigating Psychosis." IP J Surg Allied Sci 2, no. 4 (2020): 102-107. https://doi.org/10.18231/j.jsas.2020.017
