- Visibility 46 Views
- Downloads 26 Downloads
- Permissions
- DOI 10.18231/j.jsas.2023.013
-
CrossMark
- Citation
Salvaging an immunocompetent patient with extensive phycomycosis of soft tissue with single stage reconstructive surgery
Abstract
Fungal infection of soft tissue is not uncommon, and they are very well managed by anti-fungal therapy. But not all are this fortunate as extensive soft tissue involvement may be intractable to medical line of management, adverse effects of anti-fungal medications may add insult to injury thus leading to increased morbidity and mortality. Surgical help at this juncture becomes mandatory as debulking of such infected soft tissue will allow the immune system of the body to take care of the residual disease by supplementary anti-fungal therapy. Hence in such extensive involvement reconstructive surgical intervention will eradicate the disease in toto with simultaneous cover with skin graft which will be a life saver. We present here such a case scenario wherein a team approach with timely diagnosis and reconstruction helped save the life of a case.
Introduction
Management of single focus subcutaneous phycomycosis, a deep fungal infection caused by zygomatous species, [1] have mostly medical line of management as the dose required will be optimum for it to control the infection. Deep seated extensive soft tissue fungal infections are very notorious for recurrence, as anti-fungal therapy may not be sufficient to eradicate the disease.[2]
Adverse effects of antifungal medications are on many organs especially liver, kidney, and bone marrow and many cause serious life-threatening adverse effects, to eliminate such disease by medical line of management requires large, prolonged doses which are a double-edged sword.[3]
Surgical treatment of fungal infection has been controversial from quiet sometime and literature quotes not to do surgery as it may hasten the phycomycotic infection.[4], [5] We depict surgical treatment of extensive subcutaneous phycomycosis with concomitant oral KI which helped in salvaging a patient [pt].
Case History
A 22-year-old female presented to us with history of swelling of the lower back since 2 years [Figure 1]. The patient had developed fever initially for which an intramuscular injection 2 years ago was given in the gluteal region, following which she developed swelling at the injection site which spread gradually. The patient was treated as suspected abscess and a biopsy was sent, which was suggestive of tuberculosis, for which the patient was started on anti-tubercular treatment for a period of 6 months. There was no improvement in the symptoms and signs of the initial lesion and hence the patient underwent a repeat biopsy of the lesion a year later which was also sent for a culture which showed septate hyphae on KOH mount and culture grew Saksenaea vasiformis spp. The patient was started on Itraconazole (100mg twice a day) and showed minimal improvement in her general condition as well as the lesion began to decrease in size, but the patient had a flare up of the lesion on itraconazole treatment, hence she was started on saturated solution of potassium iodide (SSKI) 15 drops (TID) which was decreased to 12 drops per dose as patient couldn’t tolerate the dose. In view of the extensive nature of lesion and the adverse effects the patient was experiencing, plastic surgery team was approached for surgical excision in order to debulk the infective load.

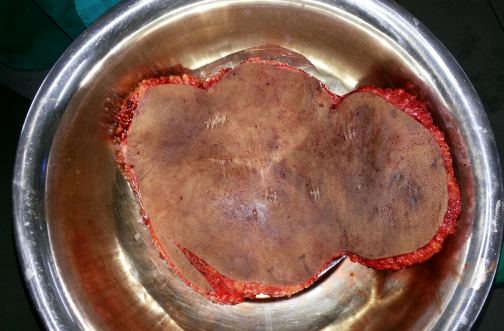

The patient was evaluated, and a CT scan was done to rule out deeper extensions or presence of any collection. After obtaining fitness for surgery, the patient underwent epifascial excision of the entire lower back soft tissue with the lesion.[Figure 2] After excision the underlying bed was found to be clear of the lesion. The excised area was then resurfaced with split thickness skin graft harvested from bilateral posterior thighs. Post operative period recovery was uneventful. Patient was started on compression garments from post operative day 20. There were no recurrences seen. Patient was continued on Itraconazole for 3 weeks and SSKI for two months. The grafts showed no breakdown during the 2 years follow up period without any recurrence of the fungal infection.[Figure 3].
Discussion
Saksenea. vasiformis found in soil is a very rare pathogen causing cutaneous infection, usually post trauma in an immunocompromised patient.[6]
Saksenaea vasiformis as described by Saksenaea in 1953,[7] is from genus Saksenaeceae, Ajello et al.[8] described the first human infection due to this species and Padhye et al.[9] reported case of subcutaneous zygomycosis of foot for which amputation of forefoot followed by a split thickness graft with concomitant potassium iodide was given.
Surgical management in such infections is controversial as literature quotes about increased mortality due to Saksenaea infection even with patients who have undergone extensive debridement.[10]
We aim at highlighting a comprehensive outlook of a few salient features of such infections from our experience of a Single stage extensive Reconstruction of subcutaneous infection where we have salvaged the patient, and we have combined with a literature review of diagnosing, treating and post operative follow up, and the importance of teamwork.
Skin involvement due to Saksenaea are very common and are only in the third place after rhino cerebral and pulmonary regions. Our case had involvement till the muscle which is rare.
In our case the initial diagnosis was missed in the first biopsy and even then, patient survived for a period of 1 year with the lesion in her skin and subcutaneous tissue which spread gradually, we attribute it to her immune competency. Surgical management in the treatment of Saksenaea is very important in order to decrease the infective load, and in areas like the back, a one stage extensive epifascial excision as done in our case will certainly eradicate the lesion.
A major drawback of extensive surgical debridement will be major loss of soft tissue and will require resurfacing with large amounts of grafts, but this problem is now mitigated by availability of reconstructive surgical skill at all major centers and hence such cases handled by tertiary care centers will bring down the mortality and morbidity. Long term follow up in patients with major reconstructive procedures, if the patient survives is also of equally important, as long-term cosmetic appearance of grafts may look unpleasant, hence compression garments and silicone gel sheeting will prevent hypertrophic scar formation. Prognosis of cutaneous S. vasiformis infections in an immunocompetent patient is better, hence an all-out attempt to eradicate the disease in toto with resurfacing must be the goal.
Conclusions
We conclude with our experience that early diagnosis with biopsy, high index of suspicion, teamwork, aggressive single stage surgical debridement of the infection with auto graft resurfacing together with systemic antifungal drug administration will lead to improved survival with a better quality of life in such a dreaded infection.
List of Abbreviations
Pt= Patient
SSKI= Potassium iodide
Source of Funding
None.
Conflict of Interest
None.
References
- Allen H. Subcutaneous mycosis. Moschella and Hurley's Dermatology. 1987;2:786-7. [Google Scholar]
- Shrestha S, Jha A, Pathak D, Kharel C, Basukala S. Ketoconazole or clotrimazole solution wash as a prophylaxis in management and prevention of fungal infection: a comparative study. Nepal Med Coll J. 2013;15(1):31-3. [Google Scholar]
- Girois S, Chapuis F, Decullier E. Adverse effects of antifungal therapies in invasive fungal infections: review and meta-analysis. Eur J Clin Microbiol Infect. 2006;24(2). [Google Scholar]
- Prasad P, Paul E, George R, Ambujam S, Viswanthan P. Subcutaneous phycomycosis in a child. Indian J Dermatol Venereol Leprol. 2002;68(5):303-4. [Google Scholar]
- Chintagunta S, Arakkal G, Damarla S, Kumar V. Subcutaneous phycomycosis presenting with multiple swellings. Indian J Paediatr Dermatol. 2016;17:58-61. [Google Scholar]
- Lamps L, Lai K, Milner D. Fungal infections of the gastrointestinal tract in the immunocompromised host: an update. Adv Anat Pathol. 2014;21(4):217-27. [Google Scholar]
- Saksena S. A new genus of the mucorales. Mycologia. 1953;45:426-62. [Google Scholar]
- Ajello L, Dean DF, Irwin RS. The zygomycete Saksenaea vasiformis as a pathogen of humans with a critical review of the etiology of zygomycosis. Mycologia. 1976;68:52-62. [Google Scholar]
- Padhye AA, Koshi G, Anandi V, Ponniah J, Sitaram V, Jacob M. First case of subcutaneous zygomycosis caused by Saksenaea vasiformis in India. Diagn Microbiol Infect Dis. 1988;9:69-77. [Google Scholar]
- Padmaja IJ, Ramani TV, Kalyani S. Cutaneous zygomycosis: Necrotising fascitis due to Saksenaea vasiformis. Indian J Med Microbiol. 2006;24. [Google Scholar]
How to Cite This Article
Vancouver
Mashalkar NS. Salvaging an immunocompetent patient with extensive phycomycosis of soft tissue with single stage reconstructive surgery [Internet]. IP J Surg Allied Sci. 2023 [cited 2025 Sep 23];5(2):55-57. Available from: https://doi.org/10.18231/j.jsas.2023.013
APA
Mashalkar, N. S. (2023). Salvaging an immunocompetent patient with extensive phycomycosis of soft tissue with single stage reconstructive surgery. IP J Surg Allied Sci, 5(2), 55-57. https://doi.org/10.18231/j.jsas.2023.013
MLA
Mashalkar, Narendra S. "Salvaging an immunocompetent patient with extensive phycomycosis of soft tissue with single stage reconstructive surgery." IP J Surg Allied Sci, vol. 5, no. 2, 2023, pp. 55-57. https://doi.org/10.18231/j.jsas.2023.013
Chicago
Mashalkar, N. S.. "Salvaging an immunocompetent patient with extensive phycomycosis of soft tissue with single stage reconstructive surgery." IP J Surg Allied Sci 5, no. 2 (2023): 55-57. https://doi.org/10.18231/j.jsas.2023.013
