- Visibility 133 Views
- Downloads 39 Downloads
- Permissions
- DOI 10.18231/j.jsas.2021.014
-
CrossMark
- Citation
Toxoplasmosis presenting as isolated cervical lymphadenopathy-A rare case
- Author Details:
-
P B Benny *
-
P K Thomas
-
Rishikesan Nair
-
M. Gowri
Abstract
Lymphadenopathy is not uncommon in toxoplasmosis. Its rare in an immunocompetent patient. We present a case of toxoplasmosis in an asymptomatic lady with isolated cervical lymph node. The diagnosis was confirmed by excision biopsy of lymph node and serology
Introduction
Toxoplasma gondii is a protozoan parasite. Infection is mainly acquired by ingestion of food or water that is contaminated with oocysts shed by cats or by eating undercooked or raw meat containing tissue cysts. Toxoplasma gondii primary infection is asymptomatic in most patients. The clinical manifestation is an isolated cervical lymphadenopathy most of the times. Prompt diagnosis and treatment requires high index of suspicion. All the differential diagnosis should be ruled out especially lymphoma before starting the treatment.
Case Report
A 22 yr. old lady presented with swelling in the neck of 1month duration. She gave no history of pain or fever. She had no history of exposure to TB patients. She doesn’t give any history of loss of weight or loss of appetite or any comorbidities. She is married and has one healthy child. She gives no history of any abortion or infertility treatment .She has a pet cat at home. On examination single discrete swelling of 2*1cm size was found in the posterior triangle of neck which was non tender, mobile and uniformly firm in consistency, . No other swelling were found elsewhere in the body. No hepato splenomegaly.

Complete blood examination, peripheral smear examination were within normal limit. Xray chest, ultra sound abdomen was found to be normal. Ultra sound neck showed single discrete lymph node in the posterior triangle of the neck
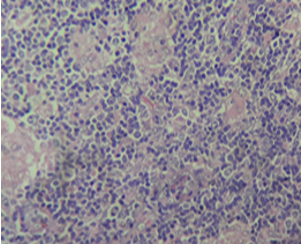
Excision biopsy was done under local anesthesia. Histopathology report came as it shows multiple microgranulomas compatible with Toxoplasma. IgG [ELISA] was 40.3IU/L. IgM (ELISA) sample absorbance ratio 6.8.
Since the patient was asymptomatic and no evidence of acute infection as per serology studies the patient is kept under follow up
Discussion
Toxoplasmosis is a zoonosis caused by toxoplasma gondii which is an obligate intracellular parasite. Toxoplasmosis remains asymptomatic in healthy individuals but may present with mild fever and lymphadenopathy mostly cervical lymphadenopathy. This has to be differentiated from other causes of cervical lymphadenopathy especially lymphomas.[1] Toxoplasmosis can produce serious manifestations in immunocompromised patient like those with malignancy undergoing chemotherapy.[2] The diagnosis of toxoplasmosis remains a difficult task as an established ideal test remains unavailable. Antibody response often peaks before clinical symptoms. IgM antibodies starts to appear within the first week of infection .it begins to peak rapidly and then starts declining to lower levels within a week or months. IgG titers appears to peak within l-2 months which will remain high but may fluctuate with time.[3]
The diagnosis of toxoplasma lymphadenitis is made by histologic examination and confirmed by serologic studies. The toxoplasma serologic profile includes IgG (dye test) and IgM antibody test, IgA, IgE, IgE immunosorbent agglutination assay and differential agglutination (AC/HS) test. In one of the recent studies, they demonstrated T gondii could be ruled out if the dye test and an IgM were negative for antibody within three months of clinical onset of adenopathy[4]
A lymph node biopsy is usually performed to differentiate malignancy from toxoplasmosis when patient presents with lymph node enlargement. The toxoplasma lymphadenitis are distinctive and often diagnostic histopathologic changes. The histopathology demonstrates a striking degree of reactive follicular hyperplasia with numerous mitoses and karyorrhectic debris in the germinal centers. Clusters of histiocytes may be observed in the interfollicular cortical and paracortical zones, and the histiocytes characteristically encroached on and blurred the margins of the reactive follicles.[5]
Since epithelioid histiocytes and prominent reactive follicles can occur in both disorders, Hodgkin’s disease and toxoplasmosis can be difficult to differentiate. The local reactional mechanism of lymph nodes to generalized infection has been described as Kikuchi’s histiocytic necrotizing lymphadenitis (KHNL), a recognized cause of lymph node enlargement. Toxoplasma infection may even mimic KHNL[6] Other causes of lymphadenitis include tuberculosis, Yersinia sp, EBV, human herpes simplex virus type 6, parvovirus B19, HIV, and systemic lupus erythematosus should also be ruled out.
The most effective medical management includes pyrimethamine and either sulfadiazine or trisulfapyrimidines plus folinic acid. The duration of therapy is usually two to four weeks for acute disease and may range to months when visceral organ involvement is encountered or when severe symptoms persist.[7] Alternative treatments include trisulfapyrimidines and sulfamethazine or sulfamethazine and sulfadiazine. All are active against tachyzoites and are synergistic in combination. Asymptomatic cases can be followed up.
Our patient probably acquired toxoplasmosis from contact with her pet which was a cat. The clinical presentation of toxoplasmosis can easily be confused with lymphoma both by clinicians and pathologists. However, after a careful history, appropriate serology, and a careful review of lymph node biopsy material, the distinction can be made between the two and unnecessary toxic therapy can be avoided
Source of Funding
None.
None.
References
- Navia BA, Petito CK, Gold JWM, Cho ES, Jordan BD, Price RW. Cerebral toxoplasmosis complicating the acquired immune deficiency syndrome: Clinical and neuropathological findings in 27 patients. Ann Neurol. 1986;19(3):224-38. [Google Scholar] [Crossref]
- Krick JA, Remington JS. Toxoplasmosis in the Adult — An Overview. Engl J Med. 1978;298(10):550-3. [Google Scholar] [Crossref]
- Hedman K, Lappalainen M, Seppaia I, Makela O. Recent Primary Toxoplasma Infection Indicated by a Low Avidity of Specific IgG. J Infect Dis. 1989;159(4):736-40. [Google Scholar] [Crossref]
- Montoya JG, Remington JS. Studies on the Serodiagnosis of Toxoplasmic Lymphadenitis. Clin Infect Dis. 1995;20(4):781-9. [Google Scholar] [Crossref]
- Mandell GL, Douglas, Bennett JE. Toxoplasma gondii. Principles and Practice of Infectious Diseases. . 1990. [Google Scholar]
- Cherin P, Ravet MBL, Aznar C, D'Oiron R, Delfraissy JF. Kikuchi's Histiocytic Necrotizing Lymphadenitis of Toxoplasmic Origin May Be Due to a Local Reactional Mechanism in Lymph Nodes. Clin Infect Dis. 1995;20(2):481-2. [Google Scholar] [Crossref]
- Herwaldt BL, Juranek DD. Laboratory-Acquired Malaria, Leishmaniasis, Trypanosomiasis, and Toxoplasmosis. AM J Trop Med Hyg. 1993;48(3):313-23. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Benny PB, Thomas PK, Nair R, Gowri M. Toxoplasmosis presenting as isolated cervical lymphadenopathy-A rare case [Internet]. IP J Surg Allied Sci. 2021 [cited 2025 Sep 22];3(2):55-57. Available from: https://doi.org/10.18231/j.jsas.2021.014
APA
Benny, P. B., Thomas, P. K., Nair, R., Gowri, M. (2021). Toxoplasmosis presenting as isolated cervical lymphadenopathy-A rare case. IP J Surg Allied Sci, 3(2), 55-57. https://doi.org/10.18231/j.jsas.2021.014
MLA
Benny, P B, Thomas, P K, Nair, Rishikesan, Gowri, M.. "Toxoplasmosis presenting as isolated cervical lymphadenopathy-A rare case." IP J Surg Allied Sci, vol. 3, no. 2, 2021, pp. 55-57. https://doi.org/10.18231/j.jsas.2021.014
Chicago
Benny, P. B., Thomas, P. K., Nair, R., Gowri, M.. "Toxoplasmosis presenting as isolated cervical lymphadenopathy-A rare case." IP J Surg Allied Sci 3, no. 2 (2021): 55-57. https://doi.org/10.18231/j.jsas.2021.014
