Introduction
Acute cholecystitis is the commonest complication of cholelithiasis. In more than 90% of patients the cause of acute cholecystitis is an obstruction of the cystic duct, mostly due to the presence of calculus or because of biliary sludge "sticking" on the neck of the gallbladder.1
With the introduction of Laparoscopic Cholecystectomy (LC), the surgical community witnessed a revolution in basic ideology and the importance of minimal access surgery.2 There are 2 schools of thought for management of acute cholecystitis-1) conservative in acute phase and posting in later (6-8weaks) for so-called interval cholecystectomy and 2) earliest cholecystectomy to all patients presenting with cholecystitis.
Although LC has now been accepted as the gold standard for managing cholecystitis with or without cholelithiasis, a similar acceptance for the management of acute cholecystitis (AC) remains controversial because of technical difficulties.3 Recently it has been also postulated that the complication when done in acute or chronic phase of cholecystitis were same.4 Benefits of this approach include reduced hospitalization, cost, decreased pain, avoidance of a large incision with improved cosmetic and reduced post-operative recovery time.5, 6 The aim of the study is to evaluate the applicability of LC in the cases presented with acute cholecystitis.
Materials and Methods
A Prospective comparative study of all the patients admitted in a tertiary care hospital between a period from October 2019 to March 2020 with acute and chronic cholecystitis who will be undergoing LC above the age of 20 years. Complete clinical details and radiological findings were recorded. Informed consent has been taken for all patients undergoing surgery. Patients unfit for general anesthesia, systemic complications like peritonitis, septicemia, Multiorgan dysfunction (MODS) were excluded from the study. Also patients less than 20 years and more than 80 years were excluded.
Data analysis
Data analysis is done by using SPSS (Statistical package for social sciences) Version 19.0. We have used Chi-square test to find the significance between acute and chronic cholecystitis with respect to qualitative data variables Mann-Whitney U test or 2 independent sample t-test used to find the significant difference between acute and chronic cholecystitis with respect to quantitative data parameters. P-value < 0.05 considered as significant.
Results
The current study included 58 cases, of which 25 presented with acute cholecystitis and 33 with chronic cholecystitis. Of the 25 cases with acute cholecystitis, 11 were males and 14 females. In the group with chronic cholecystitis, 18 cases were males and 15 were females. (Table 1)
Table 1
Sex distribution in acute and chronic cholecystitis patients.
|
Gender |
Group |
Total |
P-value |
|
|
Acute |
Chronic |
|||
|
Male |
11(44%) |
18(54.54%) |
29 |
0.596 |
|
Female |
14(56%) |
15(45.45%) |
29 |
|
|
Total |
25 |
33 |
58 |
|
25 cases with acute cholecystitis all reported abdominal pain, whereas 02 cases with chronic cholecystitis reported no abdominal pain of any sort. 58 cases under study 01 patient was having jaundice due to associated cholangitis. Fever was found to be slightly significant in the group with acute cholecystectomy. Though nausea was present in 41 cases, vomiting was reported in just 20 cases out of 58. (Table 2)
Table 2
Clinical profile of patients of acute and chronic cholecystitis
Table 3 shows there was no significant difference in the difficulty level of gall bladder removal from the GB fossa between the cases with acute versus chronic cholecystitis.
Table 3
Difficulty in removal of gall bladder in acute and chronic cholecystitis.
Of the 25 cases in the acute cholecystitis group, 21cases (88 %) did not report any postoperative complication. Two cases reported bile leaks while a subject each reported chest infection, blood in drain, vomiting and UTI. Of the 33 cases in the chronic cholecystitis group, 28 cases (93 %) did not report any complication. 4 cases complained of vomiting, 2 were diagnosed with chest infection and one subject each of blood in drain and UTI. However, the acute group showed complication of bile leak in 2 patient verses nil in chronic group. Detailed analysis is shown in Table 4.
Table 4
Complications in LC in cases of acute and chronic cholecystitis
|
Complication |
Group |
Total |
|
|
Acute |
Chronic |
||
|
Bile leak |
2 |
0 |
2 |
|
Chest infection |
1 |
2 |
3 |
|
Wound infection |
0 |
0 |
0 |
|
Blood in drain |
1 |
1 |
2 |
|
Vomiting |
1 |
4 |
2 |
|
UTI |
1 |
1 |
2 |
|
Port site hernia |
0 |
0 |
0 |
|
No |
21 |
28 |
49 |
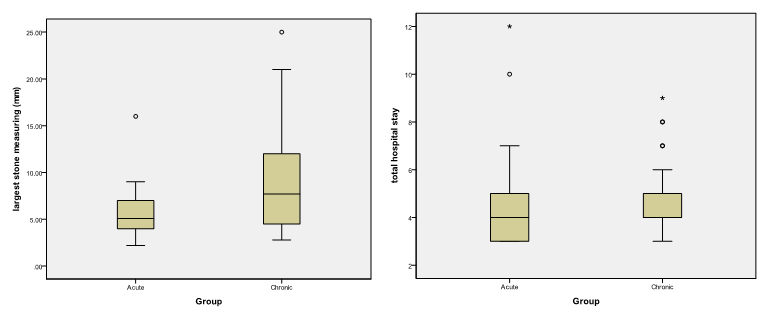
Figure 1 shows that there is significant difference between median largest stone in with acute group and chronic group.(Mann-Whitney U test, p-value < 0.05). Figure no 2 shows there is no significant difference between median total operative time in with acute group and chronic group.(Mann-Whitney U test p-value > 0.05).
Discussion
The current study included 58 cases, of which 25 presented with acute cholecystitis and 33 with chronic cholecystitis. Of the 25 cases with acute cholecystitis, 11 were males and 14 females. In contrast to our study Rexhep Selmani et al in his study noted that cholecystitis was more common in females as compared to male.7 This might be due to small size, a more number of migrating male working population in the city. All the 25 cases with acute cholecystitis reported abdominal pain, whereas 02 cases with chronic cholecystitis reported no abdominal pain of any sort. Pushpendra Malik et al.8 in their study of early and interval laparoscopic surgery in acute cholecystitis on 50 consecutive cases of acute cholecystitis noted abdominal pain was present in all 50 patients which is concordant with our study.
Of the 25 cases in the acute cholecystitis group, 21cases (88 %) did not report any postoperative complication. Two cases reported bile leaks while a subject each reported chest infection, blood in drain, vomiting and UTI. Of the 33 cases in the chronic cholecystitis group, 28 cases (93 %) did not report any complication. 4 cases complained of vomiting, 2 were diagnosed with chest infection and one subject each of blood in drain and UTI. However, the acute group showed complication of bile leak in 2 patient verses nil in chronic group that seems to be significant but this result may be bias due to small sample size. Coccolini et al9 conducted a systematic-review with meta-analysis and meta-regression of trials comparing open versus LC in patients with acute cholecystectomy and reported that the post-operative morbidity rate was half with LC (OR = 0.46) and the post-operative wound infection and pneumonia rates were reduced by LC (OR 0.54 and 0.51 respectively. Literature review showed that in several studies.10, 11, 12, 13 there was no statistically significant difference in the rate of major complications between LC in the acute phase and chronic phase.
There is significant difference between median largest stone in with acute group and chronic group by using Mann-Whitney U test p-value < 0.05 (Figure 1), which means that large stones more frequently are the cause of acute cholecystitis might be due to obstruction of the cystic duct
In our study by using Mann-Whitney U test p-value < 0.05 (Figure no 2) therefore there is significant difference between median total operative time required for LC with acute group (60 min) and chronic group (90 min), with the acute group having a lower total operative time.
In contrast, Anees et al 14 reported that a longer operative time was required for LC in the acute phase as more frequent special modifications in operative technique are needed. To avoid septic complications, the surgeon must take extra precautions, including the use of closed suction drains (80% in acute compared to 35% of delayed cases) because of the high incidence of turbid bile or even pus in the gallbladder with the potential risk of infection.
Conclusion
LC is safe in both acute and chronic cholecystitis. Our study suggests that it is advisable to operate in the acute cholecystitis that to in the 24-72 hours after the presentation of symptoms because of the better development of the plain due to edema but only by a well experienced laparoscopic surgeon. Although performing LC in acute phase had more operative difficulty and required more experience of the surgeon, but it is the demand of the time. Number of conversions to open surgery, operative time and the number of complications decrease over time as an expression of the surgeon’s learning curve. It is important that this type of surgery is performed only by experienced surgeons or under close supervision of experts. Performing the surgery successfully without any biliary injury or hemorrhage should the aim and if required for the benefit of patient conversion to open should be done.