Introduction
Acute pancreatitis (AP) is an inflammatory process of pancreas with varying involvement of regional tissues or remote organ system with an increased mortality rate.1 Around 25% of patients with acute pancreatitis develop severe acute pancreatitis (SAP) and average mortality rate in SAP is around 2-10%.2 Therefore early identification of acute pancreatitis enables rapid intervention and treatment and can improve patient’s betterment and survival. According to the 2012 Revised Atlanta Classification,3 Acute Pancreatitis identifies 2 phases of acute pancreatitis - early (First 1 or 2 weeks) and late (Thereafter). Acute pancreatitis can be either edematous interstitial pancreatitis or necrotizing pancreatitis, the latter involving necrosis of the pancreatic parenchyma and peripancreatic tissues, pancreatic parenchyma alone or just the peripancreatic tissues.Severity of the disease is categorized into 3 levels: mild, moderately severe and severe.
Severe Acute pancreatitis is defined by
Persistent organ failure for more than 48 hours involving one or multiple organs
The local complications - acute peripancreatic fluid collections, pseudocyst, acute (Pancreatic/peripancreatic) necrotic collection and walled-off necrosis.
There are numerous scoring system for prediction of severity of AP on the basis of different parameters. Ranson’s criteria and Modified Glasgow score use data that are not routinely collected at the time of hospitalisation, both require 48 hours, so early intervention is missed.4 APACHE-II basically used for ICU purpose to predict survival is complex and collection of large number of parameters makes it less favourable.5 BISAP proposed by Wu et al in 2008 is a new simple bedside prognostic score which involves routine investigation of admitted patients. BISAP is acronym for Bedside Index for Severity in Acute Pancreatitis 6. Data for BISAP score collected within the first 24 hours of hospitalization. BISAP score is an uncomplicated, quick and reasonably reliable for assessment of disease severity on admission.
Table 1
BISAP scoring system.
|
Parameters |
Score 0 |
Score 1 |
|
Blood urea nitrogen |
<25mg/dl |
>25mg/dl |
|
Impaired mental status |
Absent |
Present |
|
SIRS |
Absent |
Present |
|
Age |
<60 years |
>60 years |
|
Pleural Effusion |
Absent |
Present |
SIRS (Systemic Inflammatory Response Syndrome) is diagnosed by presence of any two of criteria:
Temperature (38c),
Pulse > 90/min,
Respiratory Rate >20 or PaCO2 <32 mmhg
WBC> 12,000/mm3 or <4,000/mm3 or >10% bands
To assess organ failure in acute pancreatitis the criteria proposed by Marshal et al Table 2. The variables are accessed at admission and again after 72 hours. A score of 2 or more in any system defines the presence of organ failure. Duration of organ failure was considered as transient for 48 hours.
Table 2
Modified Marshal scoring system for organ dysfunction.
Over past years management of AP has significantly changed. Primary treatment in early cases is non-surgical & supportive. Patients with infected necrosis with sepsis promptly requires intervention and early admission to intensive care has improved the overall outcome.7 With rising costs of intensive care treatment of acute pancreatitis and its complications there is a need for early identification of warning signs and early prompt intervention. This helps the patients to recover faster with less morbidity & mortality.8, 9 In this background, present study helps to assess the severity with few basic clinical evaluation, biochemical markers, imaging helping in early evaluation and intervention helping in better outcome of acute pancreatitis patients.
Materials and Methods
This study is a single centre, non-interventional, retrospective study conducted at Mandya Institute of Medical Sciences, Mandya, Karnataka, India, between January 2018 and December 2019, for a period of two years. Acute pancreatitis was diagnosed based on the presence of characteristic abdominal pain, raised serum amylase level three times the upper limit of normal, the presence or absence of characteristic imaging findings of acute pancreatitis and exclusion of other diseases. A total of 152 patients, both males and females presenting within 24 hours of onset of symptoms were included in study. Patients aged less than 14 years and elder patients more than 70 years are excluded. BISAP scoring is done within 24 hours of admission and data are tabulated for analysis. The scoring criteria is given in Table 1. One point is assigned for each of the variables above within 24 hours of presentation. The BISAP score ≥3 in first 24 hours is considered as predictive of severe pancreatitis.
Results
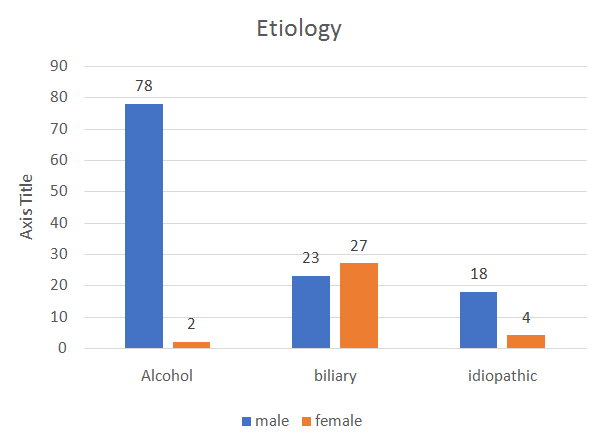
In our study Out of 152 patients, 119 were males and 33 were females (Figure 1). The youngest in the study was 17 years of age and the oldest was 67 years of age with a median age group of 42 years (Figure 2). 26% had severe pancreatitis. Acute Pancreatitis was seen in male (78%), in 4th decade (65%), alcohol was the most common aetiology (52%), followed by biliary pancreatitis (33%), remaining idiopathic (15%) pancreatitis(Figure 3). Patients with BISAP >= 3 was associated with transient or persistent organ failure and pancreatic necrosis. Accuracy to predict SAP by BISAP score was 63.3 % on the basis of sensitivity and regarding specificity it was 77.8%.
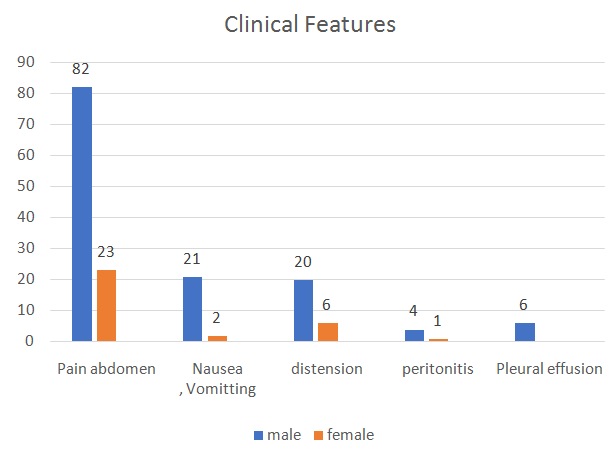
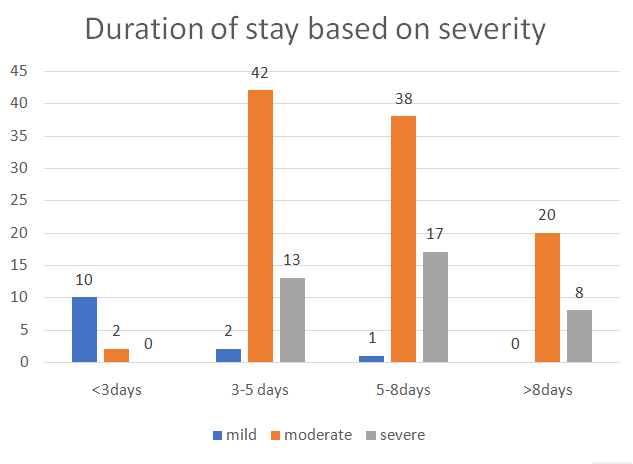
The most common presentation among these patients was pain abdomen followed by features of abdominal distension, nausea and vomiting, peritonitis and pleural effusion in the order of frequency (Figure 4). Mean duration of stay in the hospital was 9.5 days with the shortest duration being 3 days and the longest, 16 days (). 14 patients progressed to multi-organ dysfunction syndrome with shock and 32 patients had multi-organ dysfunction without shock. Complications were seen in 26% of the cases in the study with 74% having mild pancreatitis. All those with BISAP score >3 had complications. Renal failure was the most common complication (36 cases) followed by ARDS (5 cases), MODS in 2 cases and one case had cardiac failure. Transient organ failure was seen in 19 of the 26 cases. All these patients recovered without any mortality. Five cases showed persistent organ failure in our study and died due to MODS (3 cases) and ARDS (2cases) with mortality of 3%. Severity of Acute Pancreatitis was assessed based on the BISAP scoring system. Among the 152 cases, 40 cases had severe acute pancreatitis (score>3) and 112 cases had mild acute pancreatitis (score3). Organ failure was also seen in patients with BISAP >3.
Discussion
Acute pancreatitis (AP) is defined as an inflammatory process of the pancreas with possible peripancreatic tissue and multiorgan involvement inducing multiorgan dysfunction syndrome (MODS) with an increased mortality rate. 1 In western countries, gall stones are the most frequent cause of pancreatitis, in approximately 50% of patients, followed by alcohol (20%), idiopathic in 20% and other known causes in 10% cases (hypercalcemia, hypertriglyceridemia, medications, hereditary causes, sphincter of Oddi dysfunction, pancreas divisum, pancreatic neoplasms, and others). 9
The diagnosis of acute pancreatitis is based on following criteria (1) Severe abdominal pain (2) Serum Amylase or Serum Lipase more than three times higher than the institutional upper limit (3) Contrast Enhanced CT scan of abdomen finding of acute pancreatitis. In the first 72-96 hours of disease a CECT scan will often fail to demonstrate pancreatic necrosis and peripancreatic collections. A CECT scan has a place in patients who present after several days of abdominal pain when the amylase and lipase levels may have normalized or in patients with organ failure of unknown origin. Acute pancreatitis is classified clinically into mild and severe disease. Approximately 20% of patients develop severe acute pancreatitis, defined by organ failure or necrotizing pancreatitis. Severe pancreatitis is associated with a mortality of 15% to 30%, whereas the mortality of mild pancreatitis is only 0% to 1%. Organ failure is the most important determinant for mortality in acute pancreatitis. Several scoring systems can predict severe complications, but current methods of risk stratification for acute pancreatitis are complicated and require data that are not routinely collected on early stage. A new prognostic scoring system, the bedside index for severity in acute pancreatitis (BISAP), is a simple and accurate method for early identification of patients at risk of inhospital death. In this study, we evaluated the usefulness of BISAP as an early marker of the severity of acute pancreatitis. BISAP is simple to calculate, requires only physical examination, vital signs, laboratory data, and imaging for detection of pleural effusion that are commonly documented within 24 hours of presentation. BISAP predicts in-hospital death in the early stages of disease. Singh et al7 reported that patients with BISAP score ≥ 3 developed organ failure much more frequently than those with BISAP score <3. In our study, BISAP score ≥3 had a high predictive valuefor organ failure.
Conclusion
The Bedside Index for Severity in AP (BISAP) is an accurate method for early identification of patients at risk for inpatient mortality with acute pancreatitis. It is also an accurate means for risk stratification in patient with AP. The components of the BISAP Scoring System are clinically relevant and easily obtainable within 24hr of admission of the patients. The prognostic accuracy of this system is similar to those of other scoring systems.A 10% to 20% of patients experienced a severe attack of acute pancreatitis resulting in an intense inflammatory response, a variety of local and systemic complications, a prolonged hospital course, and significant morbidity and mortality.Modified Atlanta classification is a relatively objective index to evaluate both local and systemic changes in the development and progression of the disease. There are multiple scoring systems available to assess the severity of acute pancreatitis.Ranson and APACHE II scores are usually used to assess the severity of acute pancreatitis in most institutions.
A Ranson score of 3 or more or an APACHE II score of 8 or more indicates that the disease is quite severe with high chances of morbidity and mortality. BISAP is a relatively new system used to predict the severity and prognosis of acute pancreatitis. A study done by Papachristou et al.10 reported a sensitivity of 37.5%, specificity of 92.4%, PPV of 57.7% and NPV of 84.3% towards prediction of severity of acute pancreatitis.
BISAP score has several advantages to assess the severity as compared to other scoring systems. The first is that the score is simple to calculate requiring only those vital signs, laboratory investigation studies and imaging that are commonly obtained at the time of presentation or within 24h of presentation. The second is that the score was initially derived and tested using 36,248 cases of acute pancreatitis across 389 hospitals, reflecting the full spectrum of healthcare delivery.6 The third is that the score predicts in-hospital mortality.