Introduction
Hydatid cysts had been described by Hippocrates and other ancient physicians. The main causative organism is Echinococcus granulosus. The adult worm lives in the jejunum and duodenum of dogs and other canine carnivore (wolf and fox). The larval stage (hydatid cyst) is found in humans and herbivorous animals (sheep, goat, cattle and horse). The disease is prevalent in most parts of the world, though being most extensive in the sheep and cattle-raising areas of Australia, Africa and South America. It is a very significant health problem in India, owing to the favorable atmospheric as well as socio-economic conditions.1 Most of the cases in India prevail in Andhra Pradesh and Tamil Nadu with a prevalence of around 10-15%.2, 3
In human primary hydatid disease is commonly seen in the liver and lungs. These are usually seen in highly vascularized organs such as liver, lung and the spleen Involvement of osseous element is rare, with an incidence of less than 4%.4, 5 In osseous echinococcosis, spinal involvement is the most common and seen in approximately 0.2– 1% cases.5, 6 Involvement of thoracic spine is most common followed by lumbar spine.7, 8, 9 In this case report, we are presenting a lumbar spine hydatid cyst.
Case Report
Twenty one year old girl presented with low back pain and difficulty in walking from one month. The pain was gradual in onset and progressive in nature. She also complained of numbness, tingling sensation and weakness in bilateral lower limbs. There was no history of trauma to the spine. Examination revealed hypoesthesia in both the lower limbs. The deep tendon reflexes elicited were exaggerated in the lower limbs with positive Babinski sign. Magnetic resonance imaging(MRI) of the lumbosacral spine was performed. Images of the spine revealed a cystic lesion at first lumbar vertebral level which was found to be compressing the thecal sac and its components (Figure 1). On the basis of MRI report differential diagnosis of aneurysmal bone cyst and Pott’s spine were made.
Anesthetic management
The patient was evaluated pre-operatively for general anesthesia. The pre-operative assessment included complete blood count, renal function tests, liver function tests, blood sugar profile, coagulation profile, chest X-ray, electrocardiogram and covid-19 RTPCR (Reverse Transcriptase Polymerase Chain Reaction) testing along with assessment of the vitals, which further included non- invasive blood pressure, pulse rate, respiratory rate, body temperature and oxygen saturation, which were all found to be within normal limits. Patient was prepared pre-operatively after peripheral venous catheterization with anxiolytic, antibiotic and anti-sialagogue drugs. After checking the dragger machine for leak and compliance tests and ventilating the patient for 3-5 minutes, induction of anesthesia was done intravenously, using Inj. midazolam (0.1-0.4mg), inj. Fentanyl (1-2μg), inj. Propofol (2-2.5mg/kg) and inj. Lignocaine (2mg/kg). Nasal intubation with an armored endotracheal tube (ID: 7mm) was done using King Vision Video Laryngoscope using inj. Rocuronium (0.6-1.2mg/kg). Respirator was connected with a tidal volume setting of 450 ml and respiratory rate of 16 breaths/ min. Maintenance of anesthesia was done by inj. Vecuronium bromide (0.01-0.02mg/kg) at intermittent durations as required, isoflurane (1-1.5%), and O2:N2O (50:50).
Initial parameters recorded were: heart rate (HR)- 75/min, non- invasive blood pressure (NIBP)- 101/78 mmHg, oxygen saturation (SpO2)- 100% and end tidal CO2 (EtCO2)- 32mmHg.
Intra- operatively, it was found that the lesion, initially considered as an aneurysmal bone cyst or pott’s spine was found to be a hydatid cyst. As soon as the intraoperative diagnosis was established based on the gross appearance of the cyst, emergency injectable drugs (inj. atropine, inj. Adrenaline, inj. Dexamethasone, inj. Hydrocortisone, inj. Mephentermine, inj. Soda bicarbonate, inj. Deriphylline) were re-confirmed to be available in the operating room to treat an anaphylactic reaction, if presented in the patient during removal of the hydatid cyst. After necessary arrangements were made, inj. Hydrocortisone 200mg was given as a stat dose and then the lesion was extirpated with necessary precautions so as to not let the cyst fluid leak into the surrounding structures.
However, no anaphylactic reaction was encountered during the removal of the cyst and the duration of anesthesia was uneventful. The patient was successfully extubated and shifted to post-op with vital parameters measuring: heart rate (HR)- 84/min, non- invasive blood pressure (NIBP)- 108/69 mmHg and oxygen saturation (SpO2)- 100% at room air.
Surgical management
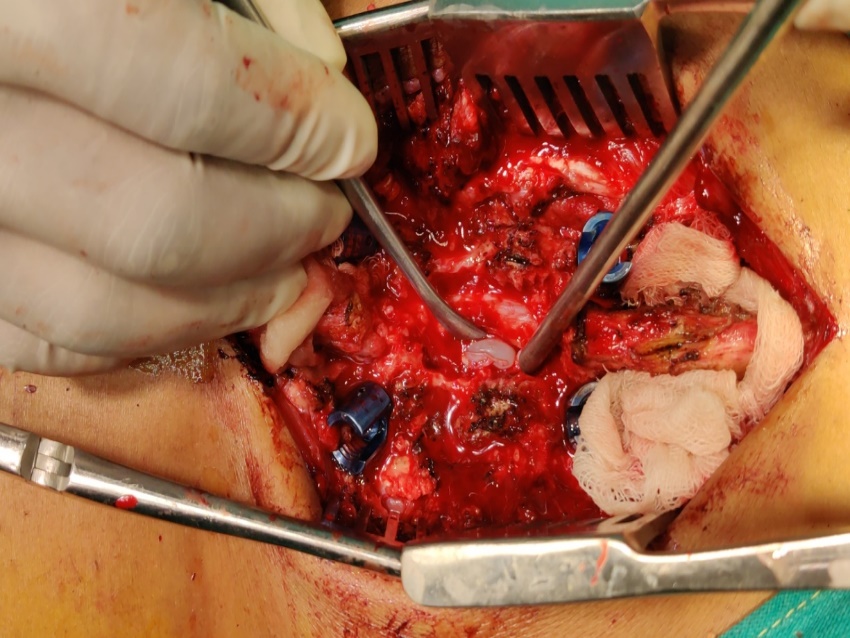
The patient was planned for transpediclular screw with rod system fixation and decompression of thecal sac. After transpedicular screws in twelve thoracic and second lumbar vertebra, laminectomy of first lumbar vertebra was performed. As an incidental finding, extradural intraspinal paravertebral hydatid cyst was encountered. With careful mopping of the surrounding structures and gentle handling, the cyst was decompressed.(Figure 2, Figure 3)
Figure 2
Extradural intraspinal hydatid cyst was seen after laminectomy which was extending through neural foramina in paravertebral region
The postoperative course was uneventful and was put on albendazole therapy. Screening for possible systemic hydatid disease was done which included computed tomography (CT) thorax and ultrasonography (USG) of the abdomen. No other system was found to be involved.
The patient was discharged after 14 days and is currently in follow-up with a significant improvement in the symptoms and no complications owing to the surgery have been noted so far.
Discussion
Hydatid disease in humans is mainly caused by larval stage of the Echinococcus granulosus. Echinococcus Granulosus has two forms, the adult and the larval forms. The larval form is found within the hydatid cyst developing inside the various organs of the intermediate host. After entering the definitive host, the scolex develops into adult worm. The worm completes its life cycle in two hosts:
Definitive hosts: dog, wolf, jackal and fox.
Intermediate hosts: sheep and cattle. Man acts as an accidental intermediate host (dead end).
In human primary hydatid disease is commonly seen in the liver and lungs. These are usually seen in highly vascularized organs such as liver, lung, brain and spleen. Involvement of osseous element is rare, with an incidence of less than 4%.4, 5 In osseous echinococcosis, spinal involvement is the most and seen in approximately 0.2– 1% cases.5, 6 Involvement of thoracic spine is most common followed by lumbar spine(24). In our case, hydatid cyst was present at lumbar spine region.
On the basis of Braithwaite and Lees study, spinal echinococcosis can be classified into five types: In type 1 the hydatid cyst is intramedullary, in type 2 the hydatid cyst is intradural and extramedullary, in type 3 the hydatid cyst is extradural and intraspinal, in type 4 the hydatid cyst is into the vertebral body, and in type 5 the hydatid cyst is paravertebral.10 In our case cyst was present extradural intraspinal region with extension into paravertebral location also. On review of literature we found only three such cases of dumbbell formation in which intraspinal hydatid cyst has an extension into paravertebral region through neural foramina.11, 12
Clinical symptoms may range from asymptomatic presentation to features due to pressure on surrounding structures depending on the anatomic location and size of the cysts.
The main radiological investigations for detection of the hydatid cysts include computed tomography (CT) and magnetic resonance imaging (MRI) but misdiagnosis is very common due to rarity of spinal hydatid cyst and it can be easily confused with pott’s spine, spinal tumors, metastasis and other cystic bony tumors of spine.13, 14
The goal of the surgery must be excision of the cyst without causing rupture. However, this is very difficult in most cases due to presence of neural roots and spinal cord with limited surgical anatomical boundaries.15, 16 In literature the widely accepted treatment of intraspinal hydatid cyst is laminectomy with surgical decompression through anterior or posterior approach and stabilization of the spine.7, 8, 17, 18 In our case we performed surgical decompression by laminectomy and partially decompressed the cyst after packing the surgical site with 3% sodium chloride solution.
The most feared and dreaded complication associated with surgical excision of hydatid cyst is anaphylaxis. The incidence of this complication varies between 1:5000 and 1:20,000 procedures and has been attributed to the Ig-E mediated type 1 hypersensitivity reaction. This highlights the anesthetic preparation in the operating room that should be at par with the possible consequences an anesthetist could face. In a prospective study, preoperative administration of the patient with H1 and H2 receptor blockers had helped to mitigate the anaphylaxis reaction secondary to the hydatid cyst- fluid spillage. Strict intraoperative monitoring should be done for signs like urticaria, bronchospasm or hemodynamic instability. No signs of anaphylactic reaction were seen in our case.




