Introduction
Ureteric calculus with a colicky pain is a common issue faced by surgeons and urologists in the ER (emergency room) and OPD (out-patient department) with a major universal health and financial strain on the health care system. Precipitation of minerals and urinary constituents such as calcium oxalate, calcium phosphate, cystine or uric acid may be a cause of ureteric calculus. It is considered a common cause of morbidity and the third most common urological disease.1, 2, 3 “There are several ureteric calculus management options, including watchful waiting, extracorporeal shock wave lithotripsy (ESWL), and ureteroscopic lithotripsy (URSL). Although now URSL is the gold standard for ureteric calculus management, but it is invasive, requires anesthesia, and these facilities in developing countries are not available everywhere. After URSL, the ureter must be stented and the stent has to be removed after a couple of weeks. They are very costly and not without post-operative complications, the key determining factor for the type of intervention remains the size of the calculus. Different studies have shown promising outcomes for ureteric calculus with medical expulsive therapy (MET) in relation to the expulsion rate and mean duration of expulsion, decrease hospital stay and less requirements of analgesics. We conduct this study to evaluate the efficacy of tamsulosin and tamsulosin plus deflazacort in the expulsion rate and expulsion time of ureteric stone and to compare the episodes of pain, duration of hospital stays, and size of calculus expelled in two groups after giving MET.
Subject and Methods
The study was conducted at the Department of Surgery, Santosh Medical College and Hospitals Ghaziabad, from November 2018 to April 2020, after obtaining permission from hospital ethical committee. This was a prospective study of one hundred patients presented during study duration in OPD or ER (emergency room) with age of greater than 18 years with symptoms suggestive of uretric calculi (colicky abdominal pain, burning micturation, increased frequency of urine, haematuria or retention of urine) & diagnosis proven by trans-abdominal USG, X- Ray KUB &/or CT KUB. Inclusion criteria was all patients presented in Santosh hospital with ureteric colic with radiographic proven uretric calculus of less than 10 mm (sub-centric). Patient of both sex with age above than 18 year. Exclusion criteria was calculi equal to or larger than 10mm, severe hydrouretero nephrosis on ultrasound examination (gross pelvicalyceal dilation with parenchymal thinning), co-morbid conditions such as diabetes, peptic ulcers, pregnancy with ureteric stone, alteration in renal parameters (serum creatinine and blood urea), previous history of ureteral manipulation and or urinary tract Surgery, urethral strictures, known sensitivities to tamsulosin and steroids, solitary functioning kidney.
All eligible patients were randomized (1:1) to two groups (A and B) by chit method each consist of 50 patients. Both group patients were received standard medical treatment such as I/V fluids, diuretics (if admitted), analgesics (drotavarine), antispasmodics (hyoscine) with advice of increase fluid intake. Group-A patient were received standard medical treatment {such as I/V fluids, diuretics (if admitted), analgesics, antispasmodics with advice of increase fluid intake} plus tamsulosin 0.4 mg once a day for 7 days. Group-B patients were received standard medical treatment {such as I/V fluids, diuretics (if admitted), analgesics, antispasmodics with advice of increase fluid intake} and tamsulosin 0.4 mg once a day plus deflazacort 30 mg once a day for 7 days.
Treatment was extended for up to a maximum of 28 days or till the passage of calculus whichever was earlier, each patient was instructed to record the date and time of calculus passage, and to pass urine through a sieve (calculus collector). Prior to study each patient underwent complete haemogram, blood urea, serum creatinine, blood sugar, urine routine and culture sensitivity, Ultrasound whole abdomen, X-Ray KUB, or CT scan KUB (if needed). After starting medical expulsive therapy all patients were advised to come for follow up on weekly interval or whenever there was uncontrolled pain or fever or on spontaneous calculus passage. Patients were asked in detail about side effects such as headache, dizziness, hypotension, retrograde ejaculation, and nausea-vomiting. All patients were subjected for examination and recommended diagnostic test.
A successful medical expulsive therapy was considered when the patient was asymptomatic, patient has passed stone, repeat imaging study does not shows any evidence of radiopaque shadow. If the patient was asymptomatic with evidence of calculus after 14 days same treatment was continued for another 14 days, medical treatment was suspended and considered failure in case of uncontrolled colic greater than two episodes, fever, progressive hydronephrosis, raised serum creatinine and patient failed to pass calculus at the end of 28 days. Patients who failed medical expulsive therapy were subjected for surgical treatment like Ureteroscopic Lithotripsy (URSL),
Table 1
Comparison of expulsion rate ofcalculus between the two groups
|
|
Group A |
|
Group B |
|
P value |
|
Expelled |
Frequency |
Percentage |
Frequency |
Percentage |
0.03 |
|
Yes |
33 |
66% |
42 |
84% |
|
|
No |
17 |
34% |
8 |
16% |
|
|
Total |
50 |
100% |
50 |
100% |
<0.05 |
Table 2
Comparison of expulsion rate according to calculus location and
size distribution between the two groups
Table 3
Comparison of side effects after MET between the two groups.
Extra-corporeal Shock Wave Lithotripsy (ESWL), and Percutaneous Nephro-lithotomy (PCNL) under appropriate anesthesia.
All the data was stored in Microsoft Excel. SPSS-17 statistics software was used for analysis. Mean and standard deviation was calculated. Comparative Analysis between two groups was done using students t- test/chi square test.
Results
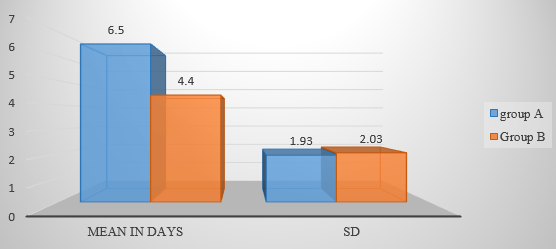
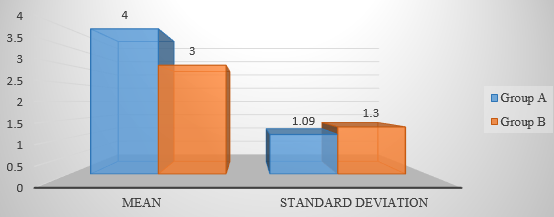
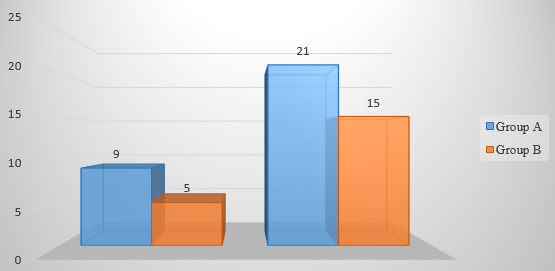
In this study totally 100 patients were equally distributed between the two groups, it was observed that in group-A, 66% of patients passed calculus successfully, while in Group-B success rate was 84%, “P” value was <0.05, (Table 1). The mean expulsion time in group-A was 6.5 days, while 4.4 days in group-B (Figure 1), “P” value was <0.05. The mean duration of hospital stay in group-A was 4 days and in group-B it was 3 days (Figure 2). It was observed that in group-A the expulsion rate of 5-7 mm calculi were 75% in both upper and mid ureter, while 97% in distal ureter (Table 2). However, in group-B expulsion rate of 5-7 mm calculi were 100% in both upper and mid ureter, while 96% in distal ureter. “P” value was 0.40. While the expulsion rate of 8-10 mm calculi in group A was 33.3% in upper ureter, 12.5% in mid ureter and 40% in distal ureter, while expulsion rate of 8-10 mm calculi in group-B in upper ureter was 50%, in mid ureter it was 33.3% while 90% in distal ureter. “P” value was 0.02. It was observed that the mean episodes of pain in first 7 days in group-A was 9 and in group-B it was 5, however mean episodes at any time in group-A was 21 while it was 15 in group-B (Figure 3). The “P” value was 0.001. Out of 100 patients 85 were admitted in which 41 were of group-A and 44 were of group-B, rest were treated on OPD basis. It was observed that in group-A, 12% had headache, 18% had dizziness, 22% had hypotension, 10% had retrograde ejaculation while 14% had nausea and vomiting. However, in group-B, 16% had headache, 14% had dizziness, 24% had hypotension, 8% had retrograde ejaculation, and 22% had nausea and vomiting. Hypotension followed by nausea and vomiting was the most common symptoms in both the groups after MET (Table 3) with “P” value of 0.69. It was observed that in group-A, 16 patients were referred for surgical management while 9 patients were referred in group-B with “P” value <0.05.
Discussion
Ureterolithiasis is a chronic condition with a major health care system burden. It mainly affects the younger populations and in developing country has a high rate of recurrence of about 50% within 5 years and 75% within 10 years.4 Previous studies have shown that calculus of less than 5 mm have a 71% to 98% chance of being expelled. The 5 to 10 mm calculus, however, has a 25% to 51% chance of spontaneous expulsion.[-5-6] It is estimated that the incidence of ureteral stones is between 1 percent and 15 percent of the population and is growing.5, 6 Among total urolithiasis, ureteral stones account for 20 percent and the lower third of ureteral stones account for 70 percent of ureteral stones and it is rising day by day.5 In general, if the patient has a ureteral calculus of 0.5 cm or less in diameter without complications, the American Urological Association panel recommended that there are more chances of spontaneous calculus elimination.6 The size and location of the stone is correlated with spontaneous expulsion of the calculus. Watchful waiting is ideal for small stones that do not cause acute symptoms and are likely to spontaneously move through, the spontaneous calculus passage depends on the calculi size, form, position, and associated ureteral edema. There is a 48 percent chance of spontaneous removal for proximal ureter calculus, 60 percent for mid-ureteral stones, 75 percent for distal stones, and 79 percent for uretero-vesical junction stones, depending on the location of the stone.4 Most passing calculus do so within 6 weeks of the onset of symptoms.7 Smaller, more distal and right-sided stones are more likely to move spontaneously,8, 5 but expectant approach may lead to complications such as urinary tract infection, hydronephrosis, and kidney function defects, the expulsion of calculi in the ureter had to be accelerated, and medical expulsive therapy came in.5 Expulsion is often impaired by the involvement of ureteral spasm, mucosal edema or inflammation and ureteral anatomy.6
We were in search of a proper pharmacological agent when we come across a symptomatic ureteric calculus appropriate for expulsion. As we all know that ureteric calculi cause ureteric edema and a steroid has anti-inflammatory actions, the pharmacological agent normally works by decreasing the tonicity of the ureter and decreasing the edema of the ureter.9 According to the 2013 European Association of Urology Recommendations on urolithiasis, for any ureteric calculus < 10 mm, medical expulsive therapy is recommended if active calculus removal is not indicated, and alpha-blockers plays a very important role for MET. Blocking these alpha-adrenergic receptors, while retaining tonic propulsive contractions, inhibits basal smooth muscle tone and hyperperistaltic uncoordinated frequency.10
In 1970 the existence of receptors in the human ureter as alpha and beta-adrenergic receptors was first identified. 11 It was shown later that alpha adrenergic receptors were categorized into three separate subtypes alpha 1A, alpha 1B and alpha 1D, of which distribution in the human ureter was alpha 1D > alpha 1A > alpha 1B.12 The alpha-adrenergic agonist has a stimulatory effect on the ureteral smooth muscles, while the beta-adrenergic receptor agonist has an inhibitory effect, whereas the alpha-1D receptors are located in abundance in the detrusor and the ureteral intramural part.13
Porpiglia et al. studied the efficacy of tamsulosin and deflazacort for the expulsion of lower ureteric calculi less than or equal to 1 cm, and found statistically significant increased calculi expulsion rates, decreased calculi expulsion duration, and decreased pain episodes compared to control. 14 In our study, we also found a statistically significant increased calculi expulsion rate, decreased calculi expulsion duration, and decreased pain episodes compared to control. Dellabella et al showed the effectiveness of tamsulosin in improving overall calculus expulsion rates whilst reducing the patient’s analgesics requirements and risk of readmission to hospital, particularly when combined with a corticosteroid (which also reduced the time of expulsion).15 In our study also the episodes of pain were less in group-B who received both tamsulosin and deflazacort in comparison to group-A received tamsulosin alone.
While six studies are presented, only three compared alpha blockers with corticosteroid to alpha blocker alone. All studies that examined corticosteroids treated distal ureteral stones only, except one study that examined all ureteral stones. Most studies included radiopaque stones only which led to a gap in knowledge about corticosteroids for non-radiopaque stones like cystine and uric acid stones. We have included all ureteral stones in our study. In this study totally 100 patients were equally distributed between the two groups, as far as the age, sex, symptoms at admission, location, and size of calculus are concerned it was observed that P value is > 0.05 which was statistically not significant.
In this study it was observed that in group-A 66% of patients passed calculus successfully, while in Group-B success rate was 84%. While study conducted by the Dellabella et al found the expulsion rate between the two groups was almost same (90% vs. 96.7%, p = 0.612).15 In group-A the expulsion rate of 5-7 mm calculi were 75% in both upper and mid ureter, while 97% in distal ureter, while the expulsion rate of 8-10 mm calculi was 3.3% in upper ureter, 12.5% in mid ureter and 40% in distal ureter. However, in group-B the expulsion rate of 5-7 mm calculi in upper and mid ureter were 100% and 96% in distal ureter, while expulsion rate of 8-10 mm calculi in upper ureter was 50%, in mid ureter it was 33.3% while 90 % in distal ureter. In our study group-B ureteric calculus were expelled maximally as compare to group-A with “P” value >0.02.
It was observed that the mean expulsion time in group-A was 6.5 days while in group-B it was 4.4 days. The mean duration of hospital stay in group-A was 4 days and in group-B it was 3 days, while, in previous studies, mean expulsion time for tamsulosin group was 5 days and 3 days for combination group, which was also significant according to Dellabella et al in 2005.15 From analysis of these data, it is evident that tamsulosin showed highest expulsion rate, less hospital stays, less mean expulsion time, and when combined with steroids (deflazacort).
“Hence for both doctors and patients, MET with tamsulosin and deflazacort has major advantages, with very mild, reasonable side effects and substantially lower healthcare system costs. MET will cause stone calculus expulsion of < 1 cm, without the need for endoscopic treatment within a few days. In addition, the use of this medication enables patients with ureterolithiasis to continue their daily activities without the need for a large number of analgesics and surgical procedures, especially in ureteric calculus smaller than 10 mm in size. MET with combination of tamsulosin and deflazacort can be recommended as an alternative to ureteroscopic removal”. MET has been shown to be cost effective by reducing the number of ureteroscopic procedures that would require following observation alone.
Conclusion
From above study, I would like to conclude that medical therapy with Alpha- adrenergic blockers (tamsulosin) is effective and have been found to increase and hasten the expulsion of ureteric calculus (of less than 1 cm in size). It also reduces mean days of expulsion, decreases pain episodes and duration of hospital stay of symptomatic ureteric calculus without complications. But, when tamsulosin is combined with deflazacort expulsion rate increases while mean expulsion time, duration of hospital stays, and episodes of pain decreases. In addition, when deflazacort is contraindicated in MET, with tamsulosin alone can also be an alternative treatment for expulsion of ureteric calculus of less than one centimeter. With few and acceptable side effects, MET with tamsulosin and deflazacort were found to be efficacious and served as an effective bridge between wait and watch management and surgical intervention. Medical expulsive therapy is proved to be efficient and should be considered for uncomplicated distal ureteral calculi less than or equal to 1 cm as the first line of treatment.