Introduction
Aspergillus species is a chronic colonizer of paranasal sinuses and ears as well as associated with a variety of different clinical conditions. Fungi are increasingly recognized as a significant cause of morbidity and mortality among the patients because of the wider use of broad-spectrum antibiotics, immunosuppressive therapy, cancer chemotherapy, increased incidence of immunodeficiency diseases and increased use of intensive care interventions.1
Aspergillosis is a mycosis of a diverse range of human and animal hosts. Aspergillus species are filamentous ascomycetes distributed primarily in soil and decaying vegetation that have an important role in recycling environmental carbon and nitrogen. Aspergillus species are thinner,septate, with regular branching and branch at acute angles. SOA is the result of extension of a primary sinonasal infection to involve paranasal structures including, but not limited to, the orbit. Lysis of the thin orbital bone allows direct communication of the nasal cavity or frontal sinuses with the orbit.2
Aspergillus species are the major etiological agents of FRS but other fungi like Schizophyllum commune, Alternaria, Curvularia and Bipolaris are also not uncommon. Histopathology is important to distinguish the invasive from the non invasive type as this differentiation helps to decide the treatment. On the basis of histopathology, FRS is categorized into non-invasive (allergic fungal rhinosinusitis, fungal ball) and invasive (acute invasive, chronic invasive and granulomatous invasive fungal sinusitis). Among the species of Aspergillus, A. flavus is more common in India and Arabian countries while in USA A. fumigatus is the most common. This difference in the species causing Fungal rhino sinusitis could be climate and geography related.3
Risk factors for invasive aspergillosis include prolonged neutropenia, transplantation, prolonged and high-dose corticosteroid therapy, haematological malignancy, chemotherapy, and advanced acquired immunodeficiency syndrome.4
Case Report
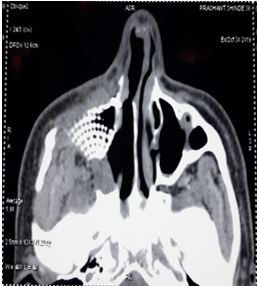
32 years old male presented with complaints of headache since 4 months, insidious in onset, progressive with no history of diurnal variation. He complained of swelling of right eye since 3 months associated with diplopia & proptosis of right eyeball since 2 months. He also presented with intermittent epistaxis from right nostril & frontal headache. There was no history of recurrent rhinitis or nasal obstruction. Patient was suffering from Hypertension & was on medications since many years. There was no history of Diabetes Mellitus. He was suffering from ankylosing spondylitis & Rheumatoid Arthritis and on immunosuppressive medications for it. Patient gave history of road traffic accident with facial trauma in past. On Examination there was proptosis of right eyeball. Grayish soft tissue was seen in the right nasal cavity. There was hypoesthesia over right maxillary sinus. CT scan of nose & paranasal sinusesrevealed a soft tissue opacification in the right maxillary sinus with right anterior ethmoid sinuses and extensive bony erosion of the sinuses and the floor of orbit. The orbit was partially sinking into right maxillary sinus. C Reactive protein levels were high (12.8).
Patient was taken up for surgery, Right Total Maxillectomy using Weber Furguson external approach was done under General anaesthesia. Intraoperative findings were suggestive of fungal debris in the right nostril, Right maxillary sinus with erosion of floor of right Orbit. It wascleared, right medial maxillectomy done. Septal cartilage was harvested. And the floor of Orbit was repaired in two layers using Septal cartilage & Titanium orbital floor implant to support the floor of the orbit. Postoperatively the infra orbital Weber- Ferguson Incision scar healed very well (Figure 1, Figure 2) Post operative CT PNS was done (Figure 3, Figure 4), radiopaque Titanium implant can visualized at the floor of right orbit.
The tissue samples from right maxilla were sent for Histopathological reporting. The reports were suggestive of chronic inflammation with extensive fibrosis, features consistent with infection of Aspergillus species which confirmed the diagnosis of Aspergillosis. Patient was given Tablet Voriconazole one tablet twice a day for 7 days followed by one tablet once a day for 3 months. Patient recovered without any comorbidity in a fellow up period of 3 months.
Discussion
Sinusitis is a common disorder affecting approxiamately 20 percent of the population at some time during their lives. Fungal sinusitis constitutes 6 – 9 % of all the rhinosinusitis. Aspergillus is the most common fungus affecting the paranasal sinuses. Overall (worldwide) Aspergillus fumigatus is the most common followed by Aspergillus flavus. Most common sinus to be involved is maxillary sinus.
The symptoms range from nasal obstruction to headache, facial pain, facial/ orbital swelling , vision disturbances, intracranial complications. Histopathogenesis of invasive aspergillosis is mainly the vascular invasion which will lead to infarction inturn leading to tissue necrosis. Invasive aspergillosis has an extremely high mortality rate, especially in immunocompromised individuals.
The diagnosis is mostly based on the tissue biopsy, fungal cultures. The aspergillus species show sepatate hyphae with branching at 45 degrees. Imaging studies include CT and MRI of PNS with Orbit and Brain. The hallmark of Invasive fungal sinusitis on CT is the bony erosion. MRI is better for the vascular invasion, soft tissue extension and cavernous sinus involvement.
The treatment modality in Aspergillosis is the prompt antifungal therapy with Surgical debridement. Voriconazole has better results and improved survival rates as compared to Amphotericin B in cases of invasive aspergillosis. Oral voriconazole has a good bioavailability and can be given in a dose of 200mg BD. Adverse effects- Visual disturbances- photopsia, Hepatotoxicity, Skin rashes, Visual hallucinations. Repeated debridements at regular intervals are performed endoscopically until freely bleeding peripheral margins are obtained. The goal of surgery is the debridement of all infected tissue within the nose and paranasal sinuses by endoscopic approach. The external approach may be inevitable when there is extensive disease of the lateral nasal wall, or evidence of orbital, facial or intracranial extension.
The combination of surgical debridement and antifungal therapy has been the cornerstone of treatment. The choice of surgical approach is dependent on the site and extent of involvement, and guided by preoperative CT and MRI imaging.5
The aim of the surgery is to provide adequate sinus ventilation by the removal of devitalized tissues and to facilitate the penetration of antifungal agents.6
Our patient was 32 years old with compliants of headache, diplopia, periorbital swelling, CT PNS revealed a soft tissue opacification in the right maxillary sinus with right anterior ethmoids and extensive bony erosion of the sinuses and the floor of orbit. The patient was taken for surgery and Right Total Maxillectomy with Right FESS done and based on the intraoperative finding of fungal debris in right maxillary sinus eroding the floor of orbit, a Titatnium orbital floor implant was used to support the floor of orbit. Morbidities like vision loss, facial deformity could be prevented due to prompt surgical intervention. In today’s era of Functional sinus surgery sometimes in such cases of aspergillosis External weber Furguson approach is very helpful for complete clearance of the disease from nose & paranasal sinuses. Also it gave good access for repiar of the floor of orbit for successful outcome of the patient without any comorbidities.
The key to reduce the mortality and morbidity in cases of invasive aspergillosis is the early diagnosis and prompt surgical intervention with medical management.
Conclusion
Invasive aspergillosis is mainly seen in immunocompromised individuals — neutropenia , uncontrolled Diabetes Mellitus ,innappropriate use of antibiotics , immunosuppressive drugs and corticosteriods , post viral infections .
The morality and morbidity like vision loss , facial deformity , meningitis, other intracranial complications can be reduced with early recognition and early intervention.
In Extensive cases External approach like Weber Furguson can be helpful for maxillectomy with almost complete clearance of disease from sinuses & nose even in today’s era of Functional endoscopic sinus surgery.
The advanced tools like Titanium plates can prevent the sinking of eyeball into maxillary Sinus & prevent morbidities like diplopia, squint & vision loss.