- Visibility 8 Views
- Downloads 4 Downloads
- DOI 10.18231/j.jsas.2022.009
-
CrossMark
- Citation
A study of splanchnic vein thrombosis in cases of acute pancreatitis and its outcome in a tertiary care center
- Author Details:
-
S Chandrashekar
Introduction
Being acute inflammatory process of Pancreas, acute pancreatitis presents with variable clinical presentation. About 80-85 percent of acute pancreatitis require only clinical monitoring and supportive care as it is self-limiting.[1], [2] About 15-20 percent evolves to moderate-severe disease leading to activation of pancreatic enzymes leading to cascade of reactions resulting in auto digestion of pancreas, necrosis, peri-pancreatic collection. These peri-pancreatic collection cause vasculitis of the surrounding vessels, external compression effects along with systemic activation of coagulation and hypercoagulable state.[3], [4], [5] This is thought to cause SVT. Management of SVT involves treatment of underlying AP and its complication like pancreatic collection. There is no clear guidelines on usage of anticoagulation and its efficacy in treatment of SVT. Spontaneous recanalization can occur in about 30% of cases of SVT.[6]
Objectives
To determine pattern of SVT, role of anticoagulation in its treatment and outcome in cases of acute pancreatitis.
Materials and Methods
Sampling Technique A serial study of 89 cases of acute pancreatitis who underwent Contrast Enhanced Computed Tomography was conducted at tertiary care centre, department of general surgery, Mysore Medical College and Research Institute, Mysore, Karnataka from the period of January 2021 to June 2021. Data related to SVT with respect to aetiology, incidence, pattern, therapy initiated, complications and outcome at the end of 3 months follow up were noted on OPD basis. Re-canalization with reduction of clot size by 75% is taken as good response. Analysis using statistics are done inference drawn.
Study type
Prospective observational study.
Inclusion criteria
Cases which presented with Acute Pancreatitis and underwent contrast enhanced computed tomography (CECT).
Exclusion criteria: Patients with
Acute pancreatitis who didn’t undergo CECT
Chronic pancreatitis
Known malignancy
Liver cirrhosis or established portal hypertension
Established prothrombotic states
The likelihood of pre-existing splanchnic vein thrombosis
Defaulters of Anti coagulation therapy follow-up
Analysis
Appropriate descriptive statistical analysis done on random samples using SPSS software, chi-square test. P values are derived with significance level of 0.05
|
|
n |
(%) |
|
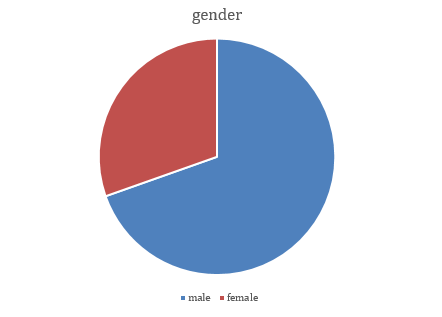
Male |
62 |
(69.66) |
|
Female |
27 |
(30.44) |
|
Ttotal |
89 |
(100) |
|
Cause |
n |
% |
|
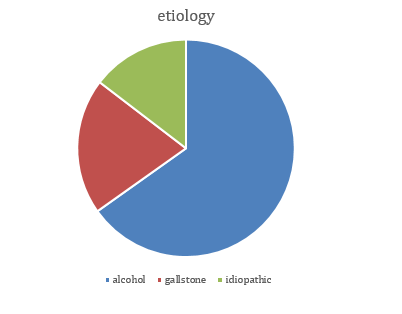
Alcohol |
58 |
65.16 |
|
Gallstone |
18 |
20.22 |
|
Idiopathic |
13 |
14.6 |
|
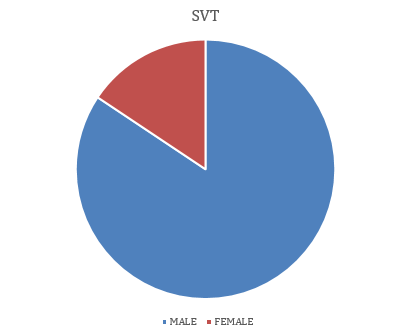
SVT-gender wise |
n |
% |
|
Male |
31 |
87.78 |
|
Female |
6 |
16.27 |
|
Thrombosis of veins |
n |
|
SVT |
4 |
|
SVT+PV |
4 |
|
SVT+PV+Portal HTN |
3 |
|
Triple vessel thrombosis |
26 |
|
|
Anticoagulant recieved |
Anticoagulant not received |
|
Reduction in Thrombus size |
27 |
3 |
|
No change |
1 |
3 |
|
Death |
1 |
1 |
|
|
Recieved Anticoagulation |
Not recieved Anticoagulation |
P value |
|
Good response |
24 |
3 |
0.0157 |
|
|
Age(Med) |
Sample size |
Anticoagulation received |
SVT in patients |
Type of study |
Main etiology |
|
Gonzelez et al.[7] |
53.5 |
127 |
4 |
20 |
Retrospective |
Alcohol |
|
Parameshwar Ramesh Junare et al.[8] |
55.41 |
105 |
12 |
24 |
Prospective |
Alcohol |
|
Lukasz Nawacki et al.[9] |
50.5 |
111 |
111 |
34 |
Retrospective |
Alcohol |
|
Present study |
39.5 |
89 |
29 |
37 |
Prospective |
Alcohol |
Results
89 Patients with acute pancreatitis were included in the present study. 56 (63%) patients were in the age group of 20-40yrs. With 62(69.66%) males and 27 (30.44%) females with mean age of 39.5 years.
Chronic ethanol consumption was the most common etiology in 65.16% (n=58) patients. Followed by gallstones as cause with 20.22% (n=18) incidence. 14.6% (n=13) had idiopathic and other cause MPD anamoly, duodenal papillae.
Among 62 males 31 had SVT (50%) and among 27 females 6 had SVT. Out of total SVT cases 87.78 % constituted male and 16.27 % constituted females. Anticoagulation (AC) therapy was considered on patients who had features of bowel ischemia (bowel wall thickening/decreased enhancement, ileus, pneumatosis), hepatic dysfunction, portal hypertension, ascites. Patients with triple vessel involvement (splenic vein, portal vein and superior mesenteric vein) and patients with portal vein thrombus of more than 50% diameter were also considered for anticoagulation.
4 patients had isolated splenic vein thrombosis, 4 patients had splenic vein + portal vein thrombosis. 3 patients had isolated splenic vein thrombosis + portal vein thrombosis along with portal vein hypertension. 26 patients had involvement of all three vessels with varied features of bowel ischemia/hepatic dysfunction. Out of 31 male patients who had SVT, 10 had past history of covid-19, out of 6 female 2 had past history of covid-19 (p<.00001).
During anticoagulation therapy, initially low molecular heparin was started for 3 days along with warfarin to keep INR in therapeutic range of 2-3. 29 patients received anticoagulation therapy during their hospital stay and were continued on oral warfarin on discharge. None of them had adverse reaction to the drugs.
Out of 29 patients who received anticoagulation, 24 showed reduction in thrombus size by 75% at end of 3 months, 3 showed reduction in thrombus size by 40-50%, 1 died due to sepsis. Of the patients who didn’t receive anticoagulation, 3 showed significant reduction in thrombus size, 3 had no significant changes, 2 died due to sepsis and shock.
Discussion
In view of limited literature available, natural history of SVT in acute pancreatitis remains elusive. Incidence of SVT is widely variable ranging from 1% to 24%. This is due to heterogeneity of the study subjects (mild vs. severe AP, acute vs. chronic pancreatitis), etiologies and imaging modality used for diagnosis (ultrasonography vs. CT scan)[10] SVT remains a frequent complication in cases of acute pancreatitis. Though the pathogenesis of SVT remains multifactorial, pancreatic and peripancreatic inflammation plays a key role. Inflammation leads to cellular infiltration, edema and systemic activation of hemostasis with consequent deposition of platelets and fibrin clot formation.[4], [5] Compression of local vessels by peripancreatic collection along with cellular disruption of pancreas leads to venous stasis and activates coagulation.[11], [12] There is also hypercoagulable state in acute pancreatitis due to increased effects of inflammatory mediators and increased synthesis of prothrombotic factors by liver resulting in SVT.[13], [14]
Limitations of the study
Patients with acute kidney injury and chronic kidney disease was not included in study as CECT is contra-indicated in them. Other modalities of imaging is not involved in the study design as they are not conventional ones in management of AP. Haemorrhagic pancreatitis is one of the contraindication for anticoagulation with LMWH. Efficacy and usefulness of other class of drugs is not analysed.
Conclusion
Splanchnic vein thrombosis is a relatively common observation in patients with severe AP; in the vast majority of patients it is associated with pancreatic necrosis and peripancreatic collections. Colocalization of peripancreatic collections and splanchnic vein thrombosis suggests that compression and perivascular inflammation are important mechanisms. Recanalization is observed in almost a third of patients, irrespectively of whether or not they receive systemic anticoagulation, and this may reflect the resolution of the AP itself and/or the drainage of adjacent collections. SVT is seen more commonly in alcohol-induced AP. It is associated with the presence of local complications of AP. AC use may not always affect the outcome. Subset of patients with SVT may benefit from AC. The role of systemic anticoagulation in splanchnic vein thrombosis associated with AP needs to be formally tested in a well-designed, prospective, randomized controlled trial.
Ethical Approval
Taken and study conducted according to the prescribed protocol. (Mysore Medical College & Research Institute) Ref. No. (EC REG: ECR/134/Inst/KA/2013/RR-19)
Source of Funding
None.
Conflict of Interest
None.
References
- P A Banks, M L Freeman. Practice Parameters Committee of the American College of G. Practice guidelines in acute pancreatitis. Am J Gastroenterol 2006. [Google Scholar] [Crossref]
- I H Mallick, M C Winslet. Vascular complications of pancreatitis. JOP 2004. [Google Scholar]
- J Easler, V Muddana, A Furlan, A Dasyam, K Vipperla, A Slivka. Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign course. Clin Gastroenterol Hepatol 2014. [Google Scholar] [Crossref]
- N A Nadkarni, S Khanna, S S Vege. Splanchnic venous thrombosis and pancreatitis. Pancreas 2013. [Google Scholar] [Crossref]
- R M Mendelson, J Anderson, M Marshall, D Ramsay. Vascular complications of pancreatitis. ANZ J Surg 2005. [Google Scholar] [Crossref]
- M G Besselink. Splanchnic vein thrombosis complicating severe acute pancreatitis. HPB (Oxford) 2011. [Google Scholar] [Crossref]
- H J Gonzelez. Splanchnic vein thrombosis in severe acute pancreatitis: a 2-year, single-institution experience. HPB (Oxford) . 2011. [Google Scholar] [Crossref]
- J P Ramesh, S Udgirkar, S Nair. Splanchnic Venous Thrombosis in Acute Pancreatitis: Does Anticoagulation Affect Outcome?. Gastroenterol Res 2020. [Google Scholar] [Crossref]
- L Nawacki. Splanchnic Vein Thrombosis in Acute Pancreatitis and Its Consequences. Clin Appl Thrombosis/Hemostasis 2021. [Google Scholar] [Crossref]
- T Dorffel, T Wruck, R I Ruckert, P Romaniuk, Q Dorffel, W Wermke. Vascular complications in acute pancreatitis assessed by color duplex ultrasonography. Pancreas 2000. [Google Scholar] [Crossref]
- J H Ranson, H Lackner, I R Berman, R Schinella. The relationship of coagulation factors to clinical complications of acute pancreatitis. Surgery 1977. [Google Scholar]
- A Lasson, K Ohlsson. Consumptive coagulopathy, fibrinolysis and protease-antiprotease interactions during acute human pancreatitis. Thromb Res 1986. [Google Scholar] [Crossref]
- A Lasson, K Ohlsson. Disseminated intravascular coagulationand antiprotease activity in acute human pancreatitis. Scand J Gastroenterol Suppl 1986. [Google Scholar] [Crossref]
- N Agarwal, C S Pitchumoni. Acute pancreatitis: a multisystem disease. Gastroenterologist 1993. [Google Scholar]
