Introduction
The treatment of lower limb tumors has shifted from amputation to limb salvage surgeries. The goal in lower limb reconstruction is maintenance of function. Function involves the need for a stable skeleton, allowing weight bearing, mobility status with adequate soft tissue coverage to nourish and protect the underlying bone. The aesthetic outcome is also important but this should never take priority over the limb’s function.
The ability of reconstructive surgeons to manage complex soft tissue defects of lower limb has advanced over the years with a better understanding of the complex vasculature within the lower extremity and advanced microsurgical techniques.
Due to availability of muscles in the thigh, flaps are easily done in this area.
The lack of local muscle flap options for the distal leg and foot makes defects in these locations challenging to reconstruct and free tissue transfers are frequently required.1
Despite the growing evidence in literature supporting advantages for use of free and vascularised pedicled flap as reconstructive options, identifying a clear recommendation has been quite controversial. In places where micro vascular expertise is not available, the pedicled flaps come to play as it is much simpler than free flaps and has a good outcome too in a resource constrained centers.
Advantages of pedicled perforator flaps include1 “Like-for-like” replacement of tissue as the donor site is in the vicinity of the defect;2 reduced donor site morbidity with preservation of the source artery and muscle and possibility of complete or partial linear closure of the donor defect;3 technically less demanding and are faster to perform than free tissue transfers.2
Aims and Objectives
To see the outcome of pedicled flaps for reconstruction after surgeries of lower limb malignant tumors.
Materials and Methods
Study design: Retrospective and prospective study.
Study population: Patients operated for lower limb malignant tumor in Dr B Borooah Cancer Institute Guwahati.
Sample size- 24.
Study period-2016-2021
Type of malignancy and stage.
Pre-operative haemoglobin, albumin.
Post-operative complication
Function of the limb.
Cosmetic outcome.
The function of the limb and cosmetic outcome of the limb was assessed by questioning patient from 4- Excellent, 3- good, 2- bad, 1- Very bad.
Exclusion criteria
Proven metastasis.
Scientific committee and Ethical committee clearance was taken.
Flaps used
Reverse sural flap
The sural artery allows probably the longest pedicled fasciocutaneous or fascial flap. Also, with the ability of being reversed, this flap can cover defects around the knee, anterior and posterior and upper third of the leg, as well as proximal foot defects. A type A fasciocutaneous flap skin flaps of up to 12 x 20cm can be raised.
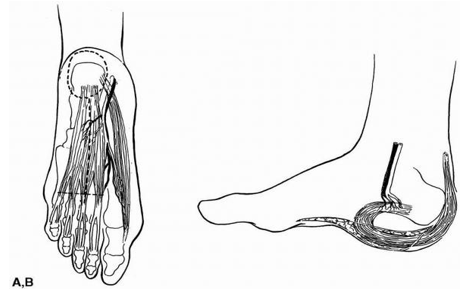
The sural neurovascular flap is a fasciocutaneous flap that is raised along the course of the sural nerve. Its blood supply depends on a constant sural artery that accompanies the nerve along its very proximal course. Distally, it depends on perforators coming from the peroneal artery. The flap is designed in the proximal posterior region of the leg, and the pivot point for this flap should be 5 cm posterior and superior to the lateral malleolus. The true pivot point was intra-operatively decided based on the direct identification, Doppler identification of perforator and put split-thickness skin graft (SSG) to cover the pedicle. The donor site was closed primarily or using SSG based on the size of the defect. A slab was given for immobilization.
Flexor digitorum brevis flap
This muscle has a relatively narrow origin from the medial process (tubercle) of the calcaneum but a substantial origin from the plantar aponeurosis. The belly gives rise to four tendons just beyond the metatarsophalangeal joints that run deep to the divisions of the plantar aponeurosis. Opposite the bases of the proximal phalanges, the tendons split to allow the passage of the tendons of the flexor digitorum longus and then insert into the sides of the middle phalanges. The neurovascular bundles to the digits and the lumbricals run between the tendons. The muscle is covered by the thick plantar aponeurosis and is flanked by the abductors hallucis and digiti minimi muscles. The neurovascular supply to the muscle arises proximally from the lateral plantar nerve and vessels as they pass laterally deep to the muscle.
The muscle is exposed by a midline incision on the plantar aspect of the foot. The plantar aponeurosis is incised and reflected medially and laterally, and the muscle is identified deep to the fascia. The musculo tendinous junctions are severed, and the muscle is turned back on itself proximally. Mobilization proceeds until the muscle covers the calcaneus, taking care not to injure the underlying lateral plantar nerve and vessels.
Figure 2
The flexor digitorum brevis and the abductor hallucis muscles are depicted with the medial plantar vessels between them. The oval dotted line indicates the excised heel ulcer, and the longitudinal dotted line indicates the incision required to expose the flexor digitorum brevis. The transverse dotted line indicates the division at the muscles and tendinous junctions. B: The muscle belly is turned on itself to cover the heel defect. 3
Medial plantar flap
It is good for distal weight bearing foot cover. The classic medial plantar artery derives its main blood supply from the medial plantar artery, a terminal branch of the posterior tibial artery.
The presence of a patent medial plantar artery should be verified using a Doppler device or arteriography. The surface design of the flap may be varied according to need. Dissection is begun distally. After the skin incision is deepened through the plantar fascia, the digital branches of the artery are divided. As dissection is carried proximally, the plantar cutaneous nerve branches are identified and separated from the medial plantar nerve by perineurial dissection and the arterial branches to the flexor digitorum brevis are divided. Finally, as the artery and nerve branches pass proximally beneath the abductor hallucis, this muscle must be divided near its insertion in order to achieve mobility of the flap. If further mobility is desired, the proximal attachments of the plantar fascia and the origin of the abductor hallucis also may be divided.
Although the base of the flap need not be wide, an effort should be made to preserve the greater saphenous vein along with its plantar tributaries. It may be necessary to mobilize the vein by dividing the dorsal tributaries. After the flap is transferred, the donor area is resurfaced with a split thickness skin graft.
Figure 3
Anatomy of the medial plantar artery.1, Medial plantar nerve; 2, medial plantar artery; 3, abductor hallucis; 4, plantar aponeurosis; 5, flexor digitorum brevis;
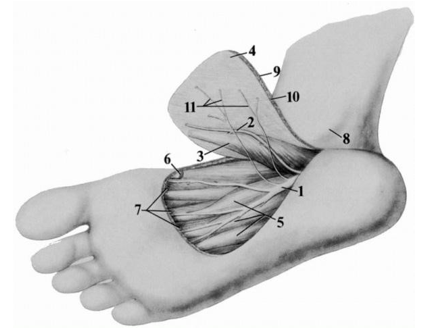
6, tendon of the abductor hallucis; 7, divided branches of the medial plantar artery; 8, medial malleolus; 9, skin; 10, subcutaneous tissue; 11, plantar cutaneous branches of the medial plantar nerve4
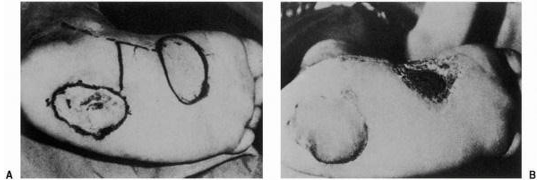
Figure 4
A: A 5 × 6-cm plantar heel defect. B: Early postoperative result using a medial plantar neurovascular island flap. (From Harrison, Morgan, ref. 2, with permission.)4
Peroneus brevis flap
The muscle flap, nearly 10 cm long by 3 cm wide, can be swung forward to cover the upper half of the lateral malleolus and the adjoining part of the fibula. A split-thickness skin graft provides the epithelial cover .There will be no functional loss using this muscle flap if the peroneus longus is preserved intact.
The distal portion of the muscle belly can be felt immediately behind the lower third of the fibula in front of the Achilles tendon. Access to the muscle is by a longitudinal incision along the posterior border of the lateral malleolus. The distal 10 to 12 cm of the muscular attachment to the fibula can be released without compromising the blood supply to the muscle flap. Having cut through the superior peroneal retinaculum, the tendon is isolated. Damage to the peroneus longus tendon with its peritendineum, situated superficial to that of the brevis, must be avoided. The peroneus brevis tendon should be transected as far distally as possible.
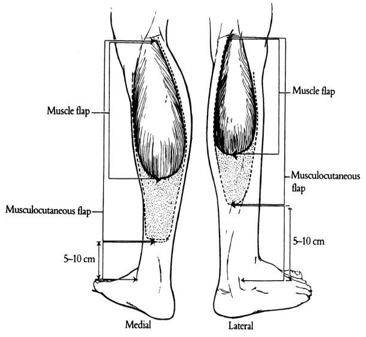
Gastrocnemius
The two origins of this muscle allow separate muscle or musculocutaneous flaps to be raised on separate pedicles, along the lateral or medial sural arteries. Useful for distal femur, proximal tibia and knee coverage, it may be advanced minimally to allow coverage over the Achilles tendon or rotated to the mid tibia thanks to anastomosis across the muscular walking are dependant on ankle plantar flexion.
Musculocutaneous Flap
The medial head of gastrinemius can support a skin flap that extends in width from the medial border of the tibia to the posterior midline of the calf. The point of rotation is the midline popliteal fossa, near the origin of the muscle and its blood supply. The level of the defect determines the length of the flap. This always includes the skin overlying the muscle and often a “random” extension of skin and subcutaneous tissue distal to the muscle. This extension is quite safely included with the flap when its length-to-width ratio is 1:1 or less. Generally, this reaches to a point approximately 10 cm above the malleolus.6
Figure 7
The potential dimensions of the medial and lateral gastrocnemius muscle (solid line) and musculocutaneous (dashed line) flaps are shown. The medial flap is larger and can be made longer than the lateral one.6
Antero lateral thigh flap
Used for defects in the thigh, maximum length and width available is 30cm and 15cm respectively. It is based in the descending branch of lateral circumflex femoral.It can be taken as fasciocutaneous and myocutaneous flap both.7
A midpoint between anterior superior iliac spine and lateral side of patella is taken. Within 3cm of radius in that point lies the perforators. A flap is raised to reach rectus femoris and vastus lateralis, rectus femoris is retracted to see the perforators and are preserved. Now the flap is raised laterally taking the vastus lateralis.Donor site is closed.
Tensor Fascia Lata
Useful as a pedicled or free flap, the thin muscle belly and long fascial extension allows this flap to be used in a multitude of scenarios, as well as it being an expendable muscle unit in the majority. Able to reach the umbilical region, perineum, ischium and groin it can incorporate skin to cover defects in the proximal lower limb, as well as iliac bone for osteomusculocutaneous coverage. It is based on the ascending branch of circumflex femoral.
The distal edge of the flap is incised first down to the fascia lata. A suprafascial dissection then continues superiorly until an ideal perforator is encountered. The rest of the flap boundaries may then be incised to create an island flap. At this point, rotation may be possible as a local flap. If necessary, the perforator can be followed through the tensor fasciae latae muscle back to its origin from the ascending branch of the lateral circumflex
femoral vessels, to extend reach and pedicle mobility, or to transfer as a free flap.7
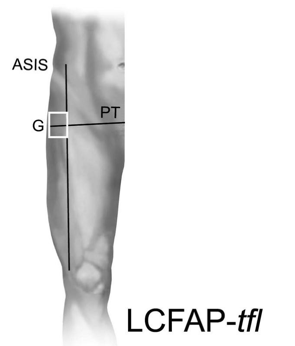
Figure 10
A perforator to the LCFAP-tfl (i.e., tensor fasciae latae) flap will be found within a rectangle with one long side corresponding to a line drawn between the anterior superior iliac spine (ASIS) and the superior lateral border of the patella, and a parallel side tangent to the anterior prominence of the greater trochanter (G). The remaining sides connect the previous pair 4 cm above and below a line drawn from the pubic tubercle (PT) to the greater trochanter (G).7
Results
Total patients: 24
Table 0
Melanoma was the most common malignancy followed by squamous cell carcinoma.
Table 0
70% patients had no post operative morbidity. There was no mortality.
Review of Literature
Lower limb soft tissue lesion pose problem for surgeons as the large post resection defect created for taking an adequate margin is large and not feasible for primary closure. Free flaps are acceptable but are complex reconstructive options.
The pioneers of plastic surgery accepted that flap design that worked well elsewhere on the body commonly failed when applied to soft tissue defects on the leg. Traditional advice was to avoid local flaps below the knee unless the defects were small or the surgeon was prepared to use special techniques such as delay incisions. Reconstructive surgeons relied on cross-leg flaps and flaps transferred from a distance using the tube pedicle technique. Ger introduced the use of transposed muscle flaps for reconstruction of the leg. Unfortunately, the area least well served by these muscle flaps is the lower third of the leg. The fasciocutaneous flap reported by Ponten showed that long narrow flaps could be safely raised below the knee as long as the deep fascia was included.8 Ponten's flaps were not based on specific perforators and therefore could not be islanded.
Following widespread use, it was realized that Ponten's flap was unsuitable for the management of difficult soft tissue defects in the lower third of the leg. Chatre and Quaba reviewed the results of 100 Ponten fasciocutaneous flaps used for lower leg reconstruction between 1981 and 1986. They reported an overall necrosis rate of 8% but the necrosis rate for flaps raised to cover defects in the lower third of the leg was an unacceptable 25%.9
The advent of fasciocutaneous flaps stimulated great interest in the cutaneous circulation of the lower extremities and in alternatives to traditional, rigid, proximally based flap designs. Of particular significance was the description of the septocutaneous vessels of the leg and the extension of the concepts of reverse flow and distally based flaps to the leg. Rather than sacrificing the whole vascular axis in the process of transferring a flap, it was soon appreciated that flaps could be based on a single septocutaneous perforator of the tibial or peroneal vessels.10 The circulation in a perforator-based flap remains more physiological compared with a distally based axial vessel-type flap.
Types of flaps
Table 2
Musculocutaneous flap classification: Mathes Nahai classification:11 Based on vascular supply
Table 3
Fascia /Fascio cutaneous flaps: 12
|
Type |
A |
B |
C |
|
Direct |
Cutaneous |
Septocutaneous |
Musculocutaneous |
|
pedicle |
|
pedicle |
pedicle |
Algorithm for lower limb flap reconstruction:12
Preoperative Evaluation
Physical examination of wound
This will involve inspecting the wound size and noting the amount of damage and loss to both the skeletal and soft tissue envelope. In addition, the vascular supply to both the area and distal regions needs to be assessed and may require the input of orthopedics, reconstructive and vascular professions.
The location of the wound also plays a large role in the feasibility of reconstruction options. The surrounding tissue also becomes important in terms of concurrent injuries, such as those in crush injuries, radiotherapy fields in malignancy, chronic infection or edema related changes.
Once the decision of surgical closure of a wound has been made, appropriate debridement must be undertaken before a final coverage option is chosen.
Patient assessment:11
Patient’s age, BMI, nutritional status, smoking status, co morbidities like diabetes causing peripheral vascular disease, pre surgery ambulatory status are important to determine rehabilitation and compliance with reconstruction.
Patient’s expectation
If given a choice most of the patient will choose limb salvage over amputation as patient want to be socially independent.
Other factors to be aware of in lower limb reconstruction include, but are not limited by:
Cost of care
Surgeon’s experience
Donor site disability
Potential complications
Multidisciplinary approach with occupational and physical therapy are required in these cases.
The various flaps available in lower limbs are –
Gluteus maximus flap
Tensor Fascia lata flap
Gracilis flap
Medial thigh flap
Lateral thigh flap
Posterior thigh flap
Sural flap
Reversed Sural flap
Saphenous flap
Soleus flap
Gastonemius flap
Supramalleolar adipofascial flap
Now –a-days due to better understanding of the anatomy of the lower limb, proplellar flaps are coming and being used.
The lower extremity is the largest donor site in the body for a perforator flap harvest. And this is why there is a very high possibility to use this option. Anatomic studies by Morris et al showed 93 perforators from the lower limb from 21 territories. There are relatively constant perforators from the 3 major vessels on the lower extremity allowing design of the propeller flaps predictable. The skin perforator flaps usually contour well because the surrounding tissue has similar thickness. It can be de-epithelialized to obliterate dead spaces; the skin laxity allows secondary procedures with ease and can have esthetically better results.
The term “propeller flap” was first used in 1991 by Hyakusoku et al.13 to describe an adipocutaneous flap based on a central subcutaneous pedicle, with a shape resembling a propeller that was rotated 90 degrees.
In 2006, combining the concept of propeller flaps and perforator based flaps, Hallock14 reported a fasciocutaneous flap that was similar in shape to the one described by Hyakusoku but was based on a skeletonized perforating vessel and was rotated 180 degrees on an eccentric pivot point. Teo15 gave the greatest contribution to the surgical technique and the application of the perforator propeller flap.
In the last years, the introduction of the propeller flaps gained great popularity; these flaps have been increasingly used for reconstruction of soft tissue defects of different parts of the body, and surgical technique has been refined and well described by several authors. Perforator propeller flaps have a reliable vascular pedicle and can undergo wide mobilization and rotation; their harvest is fast and easy and does not require microsurgery; however, accurate patient selection, preoperative planning, and dissection technique are mandatory to prevent complications.
The most common malignancy in our study was melanoma, in literature most of the flaps were done for trauma or diabetic foots.
The most common flap done in our study was the reverse sural flap for the heel defect and 1 patient among this experienced complete flap loss, the patient was diabetic and elderly female. Like any other studies our patients also had few complications like wound infection, wound gaping, partial flap loss which was managed accordingly. The most common complication in literature were partial necrosis, followed by transient venous congestion, wound dehiscence, complete necrosis, hematoma formation, arterial insufficiency vein thrombosis.16
Discussion
The sample size of the study was 24 patients.
The most common site of malignancy was in the foot, mostly heels and the most common histology was melanoma followed by squamous cell carcinoma. Wide local excision with adequate margin and nodal dissection with suitable flaps were done for all the patients. Most of the patients presented in stage II and had normal hemoglobin and albumin level.
The most common flap done was the reverse sural flap as most of the lesions were in the heel. The lesions which were smaller in size were covered using flexor digitorum brevis and medial plantar flaps.
According to Clavien Dindo 30 days morbidity mortality score, most of the patients had no complications, 6 had wound gaping, partial flap loss, wound infection which was treated with dressing and antibiotics according to the culture sensitivity. One had complete loss of flap which was treated with debridement and split thickness graft.
Functional outcome was measured by the time patient returned to work and his ability to do day to day work and scored 4-0 from excellent to very bad. Cosmetic outcome was subjective analysis of patient’s satisfaction, scored 4-0 from excellent to very bad.
Most of the patients were satisfied with both function and cosmesis. The excellent function and cosmesis were seen in 4 patients 3 of which was the Antero lateral thigh flap and 1 was medial plantar flap. 1 patient had very bad experience with unable to do daily work for >2 months and had a complete flap necrosis, she had undergone reverse sural flap.
The functional and cosmetic outcome were similar as the patients who were not satisfied with the function of the limbs were not happy with the cosmesis too.
The overall survival was 24-31 months.
Local recurrence was seen in 5 (21%) patients. It was seen as early as within 4 months ranging from 4-27 months. Distant metastasis seen in 3 patients (8%), it was seen as early as 9 months in a case of melanoma. Disease free survival was seen was 4 months in a case of melanoma.
Conclusion
The pedicled flaps have good outcome both in function and cosmesis, it can be done where plastic surgeon facilities are not available and can be reproduced with minimal morbidity especially in resource constrained centers. Pre-operative patients counselling is necessary for patient should know what to expect and be prepared for the complications ahead. It has shorter operative time compared to free flap and do not require blood vessel anastomosis expertise.

















