Introduction
One of the most often carried out procedures in developing countries is tooth extraction. The economical, general health and psychological effects of tooth loss are enormous. In fact, tooth loss has grown to be a huge global public health concern.1 Caries is frequently cited as the primary reason for extractions while discussing the indications. Periodontitis, endodontic issues, orthodontic concerns, failure of eruption, inclusion in a prosthetic treatment plan, oral trauma, aesthetic considerations, and other medical indicators that would justify treatment are also recorded. However, current summaries and projections of the proportional magnitude of causes or indicators for extractions in general, as well as causes pertaining to time, culture, and place, are insufficient.2 The loss of permanent teeth can cause masticatory dysfunction, difficulties speaking clearly, malnutrition, a lack of variety in one's diet, social isolation, and a low quality of life.3 The word quality of life (QoL) refers to a multifaceted concept relating to the patients' capacity to engage in daily activities. QOL is a term that is challenging to measure since the outcome may vary depending on how each individual interprets the data. However, the QoL surveys are made to measure the standard, efficacy, and efficiency of the treatment approaches as well as the social, psychological, and physical effects for patients with various health conditions.4 Because it is feasible to identify the requirements of the population, priorities care, and assess the effectiveness of accepted treatment techniques, QOL measurement in public health is a useful instrument for formulating welfare programmes. These assessment tools support the development of guidelines for evidence-based clinical practise by assisting researchers in evaluating the results of interventions or actions.5 The objective of this study was to evaluate quality of life among adult outpatients after non surgical extraction of teeth under local anaesthesia.
Materials and Methods
The present study was conducted among 80 patients who were above 18 years and wanted extraction of one or two teeth were included in the study. Exclusion criteria included: Patients who had systemic diseases, Patients who are on chronic NSAID therapy, Patients with contradiction of extraction under local anaesthesia and who cannot understand Questions related to quality of life, Elective surgical extraction, and difficult intra-alveolar extraction necessitating a switch to trans-alveolar extraction. Before entry into the study, written informed consent was taken from each subject. Patients’ were informed of the study’s purpose. Ethical clearance was taken. Extraction of teeth were done by the dentist under local anaesthesia (2% lignocaine with 1:80,000 adrenaline). After extraction post op instructions were given to the patients. Postoperative medication was paracetamol tablets. Patients were also instructed to report back, if ther was any increased or persistant pain in the extraction socket during post operative period. A complete questionnaire (in english, hindi and punjabi language) with information about post-op quality of life given in Table 1 below was given the patients. On day 2, 4 and 7 after extraction, patients were asked telephonically about their status. Other data included in the questions were age and sex of the patients, tooth number, intra-operative complications such mucosal tear, no complications etc., socket healing complications.
Table 1
Results
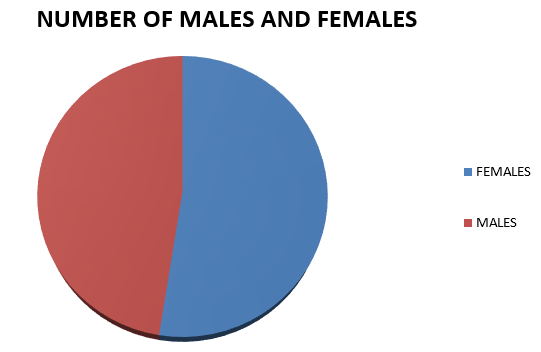
Total of 80 patients, out of which 38 were males and 42 were females (10 females were housewives and were not working) aged between 19-88 years were called telephonically on day 2, 4 and 7 after extraction and their responses were collected. The patient’s age and the sex distributions are listed in Table 2 and figure 1 below .The total number of teeth extracted was 97 (10 incisors, 8 canines, 32 premolars and 47 molars). Crown fracture and Root fracture was recorded in 15 and 8 patients respectively. 2 patients were diagnosed with acutely infected socket. The responses by the patients are given in Table 3 below.
Table 2
Sex distribution by mean age of patients
|
|
Frequency (%) |
Age range |
Mean |
Standard deviation |
|
Female |
42 (52.5) |
19-88 |
62.19 |
15.86 |
|
Male |
38(47.5) |
19-88 |
58.55 |
21.42 |
|
Total |
80 (100) |
19-88 |
60.46 |
18.67 |
Table 3
Subjects response to questions
Out of 80 patients, 76, 78, 80 patients continue to do their social activities on day 2, day 4 and day 7 respectively. 42.5% patients felt pain and swelling on day 2, but it got improved with time and only 10% of the patients felt pain during the day 4, and on day 7, no patients felt pain and swelling .Only 12.5% of the patients felt change in their physical appearance on day 2, while 3.75% of the subjects felt change in appearance on day 4. 14 and 2 patients said they felt change in mood during day 2 and 4 respectively. 12 patients and 3 patients did go to work on day 2 and day 4 respectively, but out of these 10 females were housewives and were not working already. 17.5% and 5% people said that the extraction affected their work performance during day 2 and 4 respectively. Only 6 subjects and 1 one subject took the help of somebody to do their work on day 2 and day 4 after extraction respectively. 19 patients felt difficulty in swallowing on day 2, whereas only 4 patients swallowing difficulty on day 4.Only 2 patients reported taste perception changes on day 2. The number of patients who felt changes in mouth opening were 26 on day 2 and 6 in number on day 4.Five patients had interrupted meals during day 2, and 2 patients on day 4.10% of the patients reported changes in ability to speak on day 2, whereas 7.5 % reported speech changes on day 4.6 and 3 patients had problem falling asleep in day 2 and 4 respectively. 100% of the patients had no issues on day 7.
Discussion
Immediate postoperative period following dental extraction can affect the oral health related quality of patients. According to the McGrath C, Comfort MB, Lo EC, Luo Y study's findings, there is a considerable decline in oral health-related quality of life during the first five days after third molar surgery and in the early postoperative period.6 According to reports, pain was more severe on the first day following surgery and gradually became better as the patient recovered.7 In our study we found that 42.5% of patients felt pain during day 2, but there was continuous reduction of pain with time and only 10% of patients felt pain during the day4 and no pains reported any pain and swelling during day7 after extraction.
15.8% of the patients felt change n appearance after tooth extraction in a study conducted by Adeyemo WL, Taiwo OA, Oderinu OH, Adeyemi MF, Ladeinde AL, Ogunlewe MO.8 In our present study.10 patients felt physical appearance change on day 2, whereas only 3 patients felt these change on day 4. According to a national study carried out in the United States, comorbid depression and anxiety are independently related with having 6+ teeth removed as opposed to 0–5 teeth removed. The presence of any teeth was demonstrated to be related with comorbid sadness and anxiety, but not with edentulism.9 14 patients had mood changes on day 2, while only 2 patients felt difference in their mood on day 4. On day 7, nobody felt any change in mood, according to the present study.
When evaluating the effects of these procedures on working isolation, significant findings were found. In the weeks following surgery, about 80% of patients stopped working, and their sick leave was extended by about 5 days.10 However in our study, only 15% patients discontinued their work on day 2, and 3.75% of patients did not go to work on day 4. On day 7 after simple extraction, everybody in our study went to work, except for 10 women who were housewives and did not work. The large amount of lost work resulting from the removal of the mandibular third molar, as indicated by 50 (37.0 percent) of those surveyed.11 An easy, reliable, and minimally uncomfortable approach for evaluating complaints of dysphagia or odynophagia after teeth extraction is surface EMG of swallowing. The surface EMG studies demonstrate that post-dental extraction and post-molar surgery dysphagia has an oral origin and is unrelated to the pharingeal segment and submental-submandibular muscle group. Clear EMG indicators of this form of dysphagia include a longer time between swallows, slower rate of consumption, low masseter muscle activity range, normal submental-submandibular muscle group activity range, and the "dry swallow" aftereffect.12 In our present study, 19 patients reported swallowing difficulty on day 2, and 4 patients on day 4 after extraction. On 7 day, nobody had any difficulty in swallowing.
Hotta, Mahoko & Endo, Sohei & Tomita, Hiroshi. document two examples of transient taste impairment following inferior alveolar nerve block. A 41-year-old lady was the first patient to experience this unusual anaesthetic for dental surgery problem. After receiving local anaesthetic for the removal of a left mandibular molar, she lost the ability to taste on the left side of her tongue. Three months later, she initially came to our outpatient clinic, complaining of a taste issue. Testing using electrogustometry (EGM) and a filter paper disc (FPD) revealed a taste abnormality in the left chorda tympani nerve's innervation area, as well as atrophy of the fungiform papillae on the left side of the tongue.13.Only 2 patients reported change in taste perception in our study on day 2.
As noted by Brooke, repeated punctures during the local anesthetic's infiltration might cause inflammation in this area, which then results in trismus. In addition, the volume of LA solution injected into this area may cause the medial pterygoid to stretch, which may cause this spasmodic contraction. Malamed clarified that unless the needle point mistakenly makes touch with the periosteum and becomes barbed, frequent needle punctures do not result in trismus. As a result, during retrieval, the barbed needle point shreds the medial pterygoid's muscle fibres, causing a muscle spasm that causes trismus14, 15, 16 In our present study, 26 patients and 6 patients had changes in mouth opening on day 2 and day 4 respectively. On 7 day, all the patients reported normal mouth opening.
A patient should refrain from smoking for a few days following the treatment, as well as from consuming fruit juices and hot beverages, since these activities can hinder the healing process. It is better to sip on cold water or lukewarm chamomile tea. Hard meals can occasionally be problematic. It is simpler to eat soups that aren't too hot and things like spaghetti, potatoes, and fish that can be crushed with your tongue.17 5 and 2 patients had interrupted meals on during day 2 and 4 only respectively after tooth extraction.
According to study's18 findings, patients who had their teeth pulled non-surgically did not frequently have sleep disturbance. According to Colorado-Bonnin et al., third molar extraction-related sleep disruption may be brought on by both a lengthy surgical extraction and postoperative medication-induced drowsiness. They consequently argued that patients should be informed of these side effects and how they may affect their capacity to operate machinery, including driving.8, 18 Only 6 and 3 patients had problem falling sleep on day 2 and 4 respectively after tooth extraction, in present study.
Conclusion
Simple extraction does affect the patient’s quality of life especially on day 1 and day 2 after extraction. ‘Pain and swelling felt’, and ‘change in mouth opening’ were the most affected domain. The unfavorable impact on quality of life of the patient after simple extraction was during the first two days, which decreased throughout the course of the follow up period. Patient should be told about how simple extraction might affect their quality of life in the immediate post operative period and how they can suffer alteration their daily routine.