Introduction
Around 2-14% of instances of peptic ulcer disease result in peptic ulcer perforation, a potentially fatal complication. 1, 2 This perforation causes the leakage of gastric contents into the peritoneal cavity and can be found either in the lesser curvature of the stomach or on the anterior surface of the duodenum.3 One of the most frequent reasons for urgent hospitalisation and surgery for peptic ulcer disease is perforation.4, 5
Princess Henrietta of England underwent the first clinical description of a perforated peptic ulcer in 1670.6 Since then, this sickness has claimed the lives of several well-known individuals.7 The presentation may be dramatic, with quick start, acute pain that frequently radiates to the back, and fast developing symptoms.
In this traditional presentation, the patient may remember the precise moment of perforation, which was frequently in the early morning. Pain can occasionally be sneaky.
When the perforation is tiny and the contents slowly leak into the right iliac fossa through the right paracolic gutter, it can sometimes mimic an acute appendicitis 8 and present similarly in symptoms. The indications of perforation may be subtle or ambiguous in older patients or those who have impaired immune systems.9
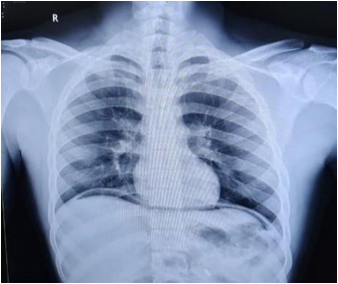
The primary differential diagnosis is an abrupt exacerbation in a patient with known peptic ulcer disease, and the diagnosis is made with a high index of suspicion.10 Often, the diagnosis is established by the presence of air under the diaphragm on an erect chest radiograph. Up to 75%[12,33]11 of erect chest radiographs contain this indicator. This indication, which can be shown on up to 75%[12,33]11 of erect chest radiographs, depends on the size of the perforation and the time after the perforation was discovered. An erect lateral chest radiograph can increase pneumoperitoneum detection by 98% and can detect as 10cc of air. 12 The current gold standard for perforation identification is the use of a computerised tomographic scan. 13, 14 While being widely available and helpful when radiation burden is a concern, ultrasonography makes pneumoperitoneum identification challenging, even for experienced sonographers. 15, 16
Materials and Methods
A prospective study of patients operated on for perforation peritonitis between March 1, 2021, and March 23, 2023 involved 104 patients with diagnosis of hollow viscus perforation with peritonititis in gastric and duodenal perforation were entered into this clinical study. Statistical comparisons were performed using the chi-square test and student’s‘t’ test. Data was analyzed for Age wise distribution, Gender wise distribution.
Inclusion criteria: All cases of hollow viscus perforation with peritonititis in gastric and duodenal perforation from age 10 to 95 years.
Exclusion criteria: Any other perforation like illeal / appendicular.
Table 1
Age distribution
|
Age in Years |
Frequency |
Percentage |
|
18-30 Yrs |
25 |
20.8% |
|
31-45 Yrs |
24 |
20% |
|
46-60Yrs |
23 |
19.1% |
|
61-75Yrs |
20 |
16.6% |
|
=/>76 |
12 |
10% |
|
Total |
104 |
100% |
Results
A total of 104 individuals had surgery for repair of gastroduodenal perforations. It was found that peptic ulcer perforation affects men more often than women since men outnumbered women by a ratio of 3.5 to 1. History of abdominal pain was present in every individual 104 in (100%), vomiting was present in 100 in (96.1%) individuals. The other complaint were fever in 84 in (80.7%), rigors in 54 (51.9%), abdominal distension in 70 (67.3%), hypotension in 49 (47.1%), tachycardia in 90 (86.5%), guarding in 99 (91.1%), rigidity in 100 (96.1%) individuals. In addition, it was been discovered that younger age groups were more susceptible to peptic ulcer perforations. In comparison to gastric perforations, the mean age of duodenal perforations was 37.75, approximately 20 years less. Over 75 percent of duodenal perforations happened before the age of 50. We highlight that gastroduodenal ulcers share a similar pathophysiology, particularly with H. pylori infestation 17 which was more prevalent in younger patients from lower socioeconomic groups, 17 despite the fact that we do not have a good reason for this shifting epidemiological profile. Since up to three out of every five patients in this research had no prior dyspeptic history, it has been shown that perforation may be the earliest sign of peptic ulcer disease. While 43% of patients reported using some kind of antiulcer medicine in the six months before to perforation.
A dry fast is likely to result in a higher frequency of difficulties within a shorter time period from the start of fasting, as opposed to the partial hunger experienced during Ramadan. As 13.5% of our patients had ulcers bigger than 2 cm in diameter, our study has demonstrated that a repair using an omental patch or simple repair delivers satisfactory outcomes even for ulcers that are rather large. Five of the nine patients who had further surgeries following the treatment were determined to have an unbroken repair. At the time of the original operation, two patients developed fibrosis around the ulcer margin, and even after the ulcer margins were removed and an omental patch was pedicled, a leakage still occurred. In our series' overall mortality of 17.3% was within the range of 4-30% that is frequently cited in numerous series.18, 19 After operative management, two of our patients succumbed to pulmonary embolism resulted in 1.9% deaths, the rest from multiple organ failure, adult respiratory distress syndrome, and septicemia.
Discussion
In this study, a total of 104 individuals had surgery to repair the gastroduodenal perforations. This results in an average of about 35 instances each year. When compared to other Eastern and Southern African series 18 and Enugu Nigeria, this number has a little higher prevalence. This may be an under representation, as numerous late cases may have passed away from the illness prior to receiving final surgery and are not included.
We discover that peptic ulcer perforation affects men more often than women since men outnumbered women by a ratio of 3.5 to 1. This result is in line with a number of previous African studies that demonstrate a male preponderance, ranging from a low of 1.3: 1 in Bugando, Tanzania 19 to a high ratios of 14.3:1 in Ido Ekiti, Nigeria 18 and 8.3:1 in Techiman, Ghana. 16 Contrary to popular belief, it is not a condition that only affects older females as shown in western television programmes. 20, 21.
In addition to the aforementioned, it has been discovered that younger age groups were more susceptible to peptic ulcer perforations. In comparison to gastric perforations, the mean age of duodenal perforations was 37.75, approximately 20 years less. Over 75 percent of duodenal perforations happened before the age of 50. The youngest patient in this series, it should be mentioned, had a stomach perforation while taking ibuprofen for a week to treat a severe low backache brought on by farm activity. Even in the past, this medication has been connected to peptic ulcers before in the paediatric age group.[32]
In contrast to other research from Nigeria that found no instances of gastric ulcer perforation,[27,30,34]22, 23 we now report that the ratio of gastric ulcers to duodenal perforations is almost 2:1. Several additional African studies demonstrate a majority of duodenal perforation, despite a prior research from a city hospital in Ghana having revealed a similar conclusion 16. We highlight that gastroduodenal ulcers share a similar pathophysiology, particularly with H. pylori infestation, 17 which was more prevalent in younger patients from lower socioeconomic groups, 24, 25 despite the fact that we do not have a good reason for this shifting epidemiological profile. Studies from Southern and Northern Nigeria show that urease culture tests for antral biopsies had a high incidence of 81.4% and over 90% with serological testing among individuals with dyspepsia. While H. pylori testing was not accessible in our facility for this investigation, all patients with perforated ulcers underwent H. pylori eradication medication. Additionally, overuse of nonsteroidal anti-inflammatory drugs, which we detected in as many as 37.5% of cases, is a significant etiologic factor, particularly in cases of stomach ulceration. Other risk variables were "dry" fasting and the use of herbal medicines that other workers have previously mentioned. Dry fasting is defined as not eating or drinking during the fast.
Since up to three out of every five patients in this research had no prior dyspeptic symptoms, it has been shown that perforation may be earliest sign of peptic ulcer disease. 43% of patients reported using any kind of antiulcer medicine in the six months before to perforation, as has been previously noted that the diagnosis of peptic ulcer illness is often made only after perforation. 26 This number is marginally higher than the 31% of perforations in individuals with established chronic peptic ulcer disease that were reported in Enugu, Nigeria. 22 When compared to an acute aggravation of a peptic ulcer, which may postpone final surgical management, this finding has the distinct benefit of raising the index of suspicion of perforation. However, with perforation, we see that discomfort remained constant throughout our series, occurring in 100% of instances and being followed by vomiting in 71% of them. This discovery is comparable to that made by Chalya et al. 19 who noted these two prominent presenting characteristics. Only 31% of our patients experience fever, making it a far less common symptom among our patients. The usage of analgesics with antipyretic effects may be to blame for this discovery.
Despite some patient were not willing or did not cooperate for computed tomographic scan at our centre during the research period, this study demonstrated a high detection rate of pneumoperitoneum of 91%. This is more than other research' predictions 11 but comparable to what was discovered in Ghana 16 As lengthy intervals between perforation and radiologic examination increase radiographic identification of pneumoperitoneum, late presentation may be a factor. 13 Multidetector CT offers the specific benefit of directly demonstrating gastrointestinal discontinuity at the location 26 and aiding in diagnosis We also propose that simple radiographs, as other workers have stated,[31] are sufficient in our environment for emergency patients with rapid onset epigastric pain to help in choosing the best surgical choice for perforated peptic ulcers.
Naturally, the bulk of our patients belonged to lower socioeconomic classes in a rural town like ours. However, the clergy or pastors were another risk category identified by this study. Over a five-year span, four pastors who had perforated peptic ulcers had surgery. They were all male and had gastrointestinal perforations. Before they had perforation, they had been dry fasting for three to seven days.
Two other female patients, one with a stomach perforation and the other with a duodenal one, were also hospitalised with symptoms. Both admitted with symptoms while one who was fasting, suffered with stomach perforation. Peptic ulcers and their consequences are more common during the Ramadan fast, according to several studies in the past A dry fast is likely to result in a higher frequency of difficulties within a shorter time period from the start of fasting, as opposed to the partial hunger experienced during Ramadan.
As 13.5% of our patients had ulcers bigger than 2 cm in diameter, our study has demonstrated that a repair using an omental patch or simple repair delivers satisfactory outcomes even for ulcers that were rather large. Five of the nine patients who had further surgeries following the treatment were determined to have an unbroken repair. At the time of the original operation, two patients developed fibrosis around the ulcer margin, and even after the ulcer margins were removed and an omental patch was pedicled, a leakage still occurred. Our series' overall mortality of 17.3% is within the range of 4-30% that is frequently cited in numerous series. 27
After reoperations, two of our patients succumbed. Pulmonary embolism resulted in 1.9% deaths, the rest from multiple organ failure, adult respiratory distress syndrome, and septicemia.
Conclusion
We state in conclusion that, the perforated peptic ulcer is a prevalent surgical issue in contemporary society. The majority of these perforations are gastroduodenal in nature, and for most patients, they constitute the initial indication of peptic ulcer disease. To determine the diagnosis in this case, a simple chest radiograph in the classic case of sudden onset epigastric pain is enough.