Introduction
Facial injury is devastating physically as well as psychologically. One of the most rewarding and demanding aspects of dental and surgical practice is the management of a patient who has suffered facial trauma.1
The angle of the mandible is the second most frequent region for fractures caused by alleged assaults and the third most fractured region in case of falls. Due to the change in the lines of calcification and strength from the horizontal body to the vertical ascending ramus, the mandibular angle is a preferred region for fractures. Additionally, impacted or partially erupted third molars are found in the mandibular angle. Bezerra et al. and Iida et al. reported that the presence of third molars multiplies (up to 200%) the risk for an angle fracture.2
The management of trauma has evolved greatly over the years which started from supportive bandages followed by semi-rigid to rigid fixation. Towards the end of the 1980’s, a clear change appeared in fracture treatment. In the course of this decade, the type of osteosynthesis changed from wire and miniplates to compression plates and lag screws.3
The mandibular angle fracture treatment is done to restore the anatomical form and function with particular care to establish the occlusion. Treatment of mandibular angle fractures requires a thorough understanding of the surgical anatomy, muscle insertion, biomechanical forces at the angle region, importance of occlusion and the presence of third molar in the line of fracture. The ideal method of treatment of mandibular fractures should have the objectives of perfect anatomical reduction, stable fixation and painless mobilization of the injured region around its articulation (Gear et al., 2005).4
Current practice uses a variety of combinations of trans-orally placed small plates secured with mono-cortical screws for fixation of angle fractures. A decade ago, two point fixations with miniplate and mono-cortical screws for angle fractures was popular, but was found to have a much higher complication rate when compared with one point fixation. Hence, the single miniplate has become the standard technique for angle fractures in many units.5
According to Ellis et al (1996) Lag screw fixation is a safe effective and inexpensive method that has number of advantages over plate osteosynthesis. The principle of lag screw is based on axial compression between the fragments. The screw glides through the fragment located near the screw head and seize the fragment located distant from the screw head. Less implant material is required in lag screw technique as compared to miniplate technique. Besides supplying compression between the fragments to support healing, fracture stabilization is firm and tissue exposure is reduced and it can be applied more rapidly.6
Even though lag screw technique is not widely used now days but because of its number of advantages like ability of compression osteosynthesis of fragments and its rapidity, we are doing a study to evaluate osteosynthesis of miniplate versus lag screw in the management of mandibular angle fracture.
Materials and Methods
The study was a controlled, randomized, single-blind, parallel group study that was conducted on 30 patients (49 males and 51 females; mean age 26.3±7.06 years) with the inclusion criteria as: patients with isolated mandibular angle fracture / multiple fractures of mandible involving the angle, patients willing for follow up & patients who come under ASA I category. The exclusion criteria were: Comminuted fractures of mandible, fractures in pediatric mandible, fractures in edentulous mandible, Patients not willing to return for follow up & ASA III, IV, V Category patients.
This study was approved by the Bapuji Dental College & Hospital IRB and all participants signed an informed consent agreement. After obtaining ethical and research committee approval, informed and written consent were obtained, patients of both genders with isolated mandibular angle fracture or multiple fractures involving angle of mandible was included. We confirm that we have read the Helsinki Declaration and have followed the guidelines in this investigation. Patients were divided in to two groups of 15 each randomly for managing angle fracture of mandible. Group-1 (miniplate group) patients undergoing treatment of angle fracture of mandible using standardized miniplate (orthomax system) and Group-2 (lag screw group) patients undergoing treatment of angle fracture of mandible using lag screw (orthomax system). The method of randomization was a simple coin toss by which the patients were allotted to either Group-1 (miniplate group) or Group-2 (lag screw group).
A standardized data sheet was formulated and demographic variables and relevant clinical and radiological finding were noted. Procedures were carried out under general anesthesia with strict aseptic precautions. A 4 holed stainless steel standardized miniplate (orthomax system) with bar was used for one group. The thickness of plate was 2 mm. The length of screws were 8mm, width 2mm, diameter at head was 3mm and height of the head was 1mm and a standardized lag screw (orthomax system) of 4 mm diameter at head, height of head was 1mm and length varies between 20mm to 26 mm was used for the other group.
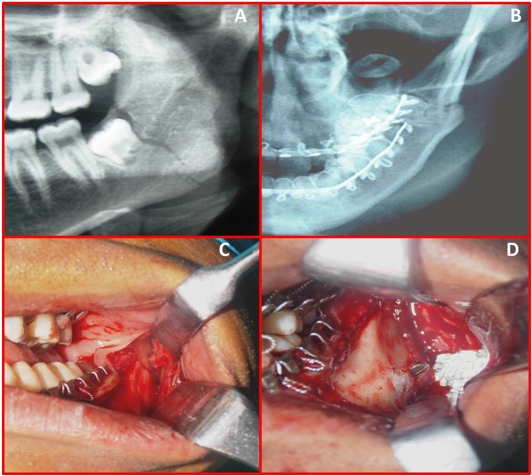
In Group-1 (miniplate group) an appropriate intraoral/extra oral incision was selected. Fracture site was identified, reduced, and after obtaining satisfactory occlusion, temporary maxillomandibular fixation was placed using either Erich’s arch bar or Ivy loop eyelet wiring. Fixation was done using standardized miniplate. In Group-2 (lag screw group) an intraoral vestibular incision from premolar region to retromolar region was given to visualize fracture line. The occlusion was restored and fragments were anatomically coapted by manual repositioning. The hole was drilled caudolateral to craniolingual. When bore in distal fragment was finished. A hole was drilled further along predetermined axis into proximal fragment until it penetrates the inner cortical bone. After the holes in both fragments are finished, depth gauge was then used to determine the length of screw required a suitable bone screw was now used. By firmly tightening screw, fracture surfaces were stabilized under pressure. The lag screw runs obliquely through body of mandible in anteroposterior direction. It enters the body approximately in the region of 1st molar at the level of external oblique ridge and exit medially, anterior to the mandibular foramen. After fixation entire duration of fixation for plate, lag screw from drilling in bone to complete fixation was recorded and noted in case history preform. Closure was then done 7 patients were extubated and sent to the recovery room. Patients in either group were hospitalized for at least 5 days and were given I.V. antibiotics and analgesics for at least 5 days. Patients in either group were advised to be on a strict liquid diet for 4 weeks post-operatively. All the patients were followed up postoperatively for at least 8 weeks at which point the arch bars were removed and were assessed clinically and radiographically. (Figure 4, Figure 5, Figure 6) Patients were evaluated for primary bone healing over 8 week post operatively. All the patients were followed for a period of 2 months at the interval of 1 week, 2 weeks, 4 weeks, and 8 weeks by an experienced oral surgeon. All patients were evaluated for the following criteria:- Radiological evaluation of reduction and fixation, Postoperative occlusion, Infection and Segmental mobility. Data was collected and tabulated using Microsoft Excel and statistical analysis of results were performed using SPSS software 16.0 version. The test used for analysis was paired t test. Results were considered statistically significant if P < 0.05.
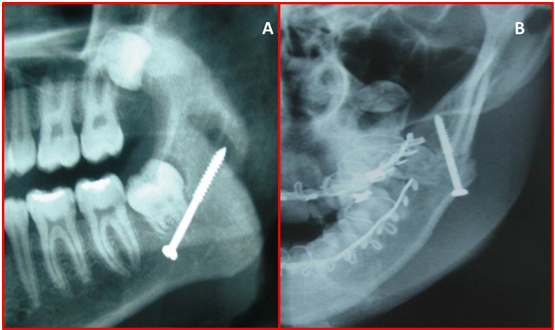
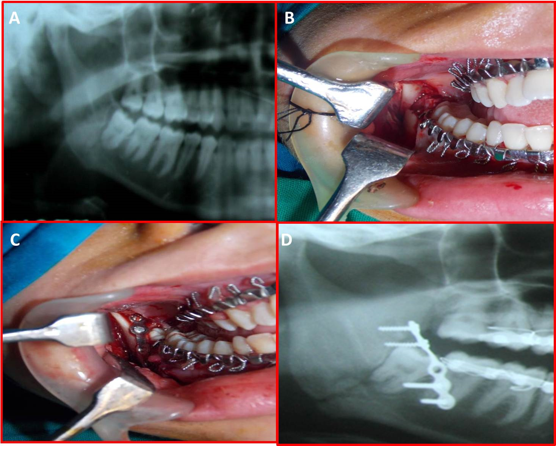
Figure 4
A patient treated with miniplate fixation. A) Radiograph showing Mandibular Angle Fracture. B) Intra Oral Exposure of Mandibular Angle Fracture. C) Intra Oral Miniplate Fixation. D) Post-Operative Radiograph
Results
The demographic data was recorded from all the patients and it was found that the patients with mandibular angle fractures range from 20-39 years with mean age of 28.40 years in miniplate group and 26.86 years in lag screw group with increased incidence of fractures between 16-30 years, with 90% male predominance. A satisfactory reduction and occlusion was achieved in all the patients. Antibiotics were continued in all the patients for a period of 5-7 days post operatively. Third molar were present in 90% of the cases in the line of fracture and were removed in 5% of the patients at the time of surgery.
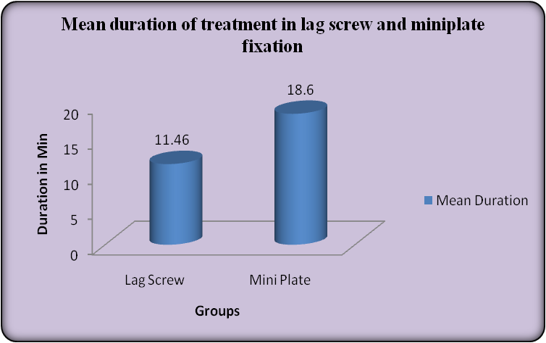
In Group 1 (miniplate group) mean duration of fixation was 18.46 min and in Group 2 (lag screw group) mean duration of fixation was 11.46 minutes. It was found that lag screw fixation takes less time than miniplate fixation (Table 1) (Figure 1).
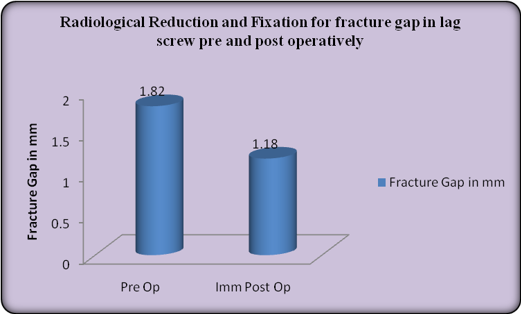
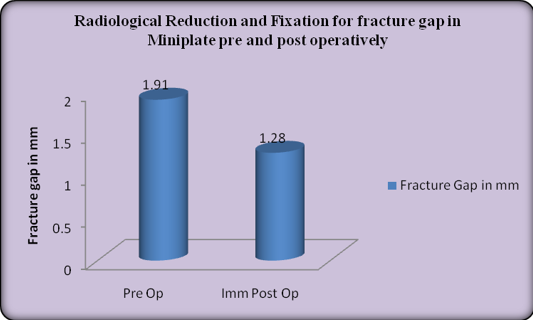
In Group 1 (miniplate group) mean fracture gap preoperatively and in Group 2 (lag screw group) was found to be 1.91 mm and 1.82 mm respectively. Immediate post operatively fracture gap was reduced to 1.28 mm and 1.18 mm respectively and at the 8th week follow-up the gap was completely obliterated (Table 2) (Figure 2).
In Group 1 (miniplate group), 3 patients (20%) presented with infection at the 3rd week follow-up. During 4th week follow up four patients (26.66%) in Group 1 (miniplate group) and one patient in Group 2 (lag screw group) presented with Infection. In Group 2, infection might be due to poor oral hygiene, mild segmental mobility and screw loosening. Most of the patients were managed with antibiotics and 2 (13.33%) patients in Group 1 (miniplate) required plate removal at 3 months follow-up due to the infection and malocclusion (Table 3) (Figure 2).
In Group 1 (miniplate group) 20% of the patients presented with unstable fracture fragments with mild segmental mobility in 1st week follow up. 13.33% patients show mild segmental mobility in 2nd week follow up. During 4th and 8th week follow up all patients showed stable fracture fragments with no segmental mobility. In Group 2 (lag screw group) none of the patient presented with segmental mobility till 8th week follow-up, all the patients (100%) showed stable fracture fragments. but overall there was no statistical difference between the groups, p value ~ 0.31. In Group 1 (miniplate group) total of 5 patients presented with segmental mobility in 1stand 2nd week post operatively. All the patients in this group were successfully subjected to 4 weeks of IMF using wires. No cases of fibrous union or non-union were noted in our study in both the groups (Table 3) (Figure 3).
60% of the patients in Group 1 (miniplate group) and in 26.66% of the patients in Group 2 (lag screw group) presented with mild occlusal discrepancy at immediate post-op. 13.3% of patients in Group 1 presented with mild occlusal discrepancy in 2nd and 4th week follow up which was corrected by using guiding elastics 24 hour/day for a period of 2 weeks. During the 8th week follow-up all the patients had satisfactory occlusion (Table 3).
Table 1
Duration of fixation
|
Group |
Mean Duration |
SD |
t value |
p value |
Significance |
|
Lag Screw |
11.46 |
1.684 |
14.717 |
0.000 |
HS |
|
Mini Plate |
18.60 |
0.828 |
Table 2
Radiological evaluation of reduction and fixation for fracture gap preoperativelyand immediate post operatively with in using paired t test
|
|
Stage |
Fracture Gap in mm |
SD |
t value |
p value |
Significance |
|
Lag Screw |
Pre Op |
1.82 |
0.165 |
19.000 |
0.000 |
HS |
|
Immediate Post Op |
1.18 |
0.130 |
||||
|
Miniplate |
Pre Op |
1.91 |
0.135 |
20.873 |
0.000 |
HS |
|
Imm Post Op |
1.28 |
0.147 |
|
|
Table 3
Number of cases with infection, segmental mobility and post-operative occlusion in lag screw and miniplate group.
Discussion
The strategic position of the mandible on the facial skeleton and its unique role in mastication, deglutition, phonation and aesthetics compels the clinician to give immediate attention whenever it is fractured.1, 2
Maxillomandibular fixation remains an important and effective tool especially in cases where plates cannot be used due to economical, personal and logistic reasons. Research continues to focus on the size, shape, number and biomechanics of plate/screws systems to improve surgical outcomes.
This study was conducted to compare the efficiency of lag screw with that of the standard miniplate in the treatment of mandibular angle fractures. According to Ghali G.E. et al lag screw fixation is the best means of providing compression and load sharing across the fracture site because all fixation forces are directed across the long axis of screw and there is no metal to metal friction points, lag screws obtain and retain stability better than any other mode of fracture fixation.7
In the study done by Ellis E et al the time needed to place lag screw is less as compared to plate, according to them fixation of screw is much faster than the adapting and securing the bone plate at fracture site.8 In our study mean duration of fixation in group 1(miniplate group) was 18.46 min and in group 2 (lag screw group) mean duration of fixation was 11.46 minutes. It was found that lag screw fixation takes less time than miniplate fixation.
According to Abdelfadil E et al rigidity of fractured segments produces a stable foundation for soft tissue growth and provides improved vascularity to the area and allows better healing of wound. It also prevents bacteria from being continually pumped through the fracture site thereby decreasing the chance of osteitis. It is seen that greater the mobility present at the fracture site, higher the chances of infection. For a successful treatment, the osteosynthesis device must provide adequate stability which controls the inter-fragmentary movements without necessarily preventing it. It has been proved that though the miniplate system is semi-rigid, this amount of rigidity is sufficient for effective osteosynthesis of fractures and to resist masticatory forces during the period of healing.[38] In our study 20% of the patients presented with unstable fracture fragments with mild segmental mobility in 1st week follow up and 13.33% patients show mild segmental mobility in 2nd week follow up in Group 1 (miniplate group). In Group 2 (lag screw group) none of the patient presented with segmental mobility till 8th week follow-up, all the patients (100%) showed stable fracture fragments. but overall there was no statistical difference between the groups (p value = 0.31).
In Group 1 (miniplate group) total of 5 patients presented with segmental mobility in 1stand 2nd week post operatively. All the patients in this group were successfully subjected to 4 weeks of IMF using wires. No cases of fibrous union or non-union were noted in our study for both the groups. The results of our study for either group were in accordance with studies conducted by various authors who found no case of nonunion or fibrous union very similar to that in our study.9
Mandibular angle fractures are known to be associated with a higher post-operative infection than any other type of fracture. The incidence has been reported to be as high as 32%. The post-operative infection might be due to contamination, presence of tooth in the line of fracture, and also related to reduced stability of the fracture fragments. Stability is considered as the best protection against infection, as movement in the presence of foreign bodies (i.e. loose screws) usually leads to infection.
In Group 1 (miniplate group) 3 patients (20%) of the patients presented with infection at the 3th week follow-up. During 4th week follow up 4 (26.66%) patients in Group 1 (miniplate group) and one patient in Group 2 (lag screw) presented with infection. All patients responded well to the use of oral antibiotics and local wound care with regular saline and betadine irrigations. A single patient in Group 1 (miniplate group) developed an extra-oral draining fistula at 4 weeks post-operatively that required incision and drainage with extended period of antibiotics and healed uneventfully over a period of 4 weeks and in Group 2, might be due to poor oral hygiene, mild segmental mobility and screw loosening. Most of the patients were managed with antibiotics and 2(13.33%) patients in Group 1 (miniplate) required plate removal at 3 months follow-up due to the infection and malocclusion. The results of our study are comparable to the study done by Levy et al in 1991 who reported 19 angle fractures treated with single miniplate placed across the oblique line and found 15.7% infection and 5.3% malocclusion.10
Restoration of the pre-morbid occlusion is one of the most important goals of management of fractures of the dentofacial region. In our study, 60% of the patients in Group 1(miniplate group) and in 26.66% of the patients in Group 2 (lag screw group) presented with mild occlusal discrepancy at immediate post-op. 13.3% of patients in Group 1 presented with mild occlusal discrepancy in 2nd and 4th week follow up which was corrected by using guiding elastics 24 hour/day for a period of 2 weeks. During the 8th week follow-up all the patients had satisfactory occlusion. The presence of occlusal discrepancy post-surgery depends on patient’s dental status, the number of fractures, type of fractures, the degree of displacement of fragments, type of reduction, type of immobilization and the time of immobilization. Many early occlusal irregularities result from muscle guarding and “posturing” of the mandible by the patient and these resolve spontaneously. The use of a single miniplate at the angle region is a simple and reliable technique but it leads to opening of the fracture line at lower border and lateral displacement of the fragment at the inferior border and posterior open bite at the fracture site.11
Biomechanical analysis by Kroon et al. demonstrated that when an occlusal load was placed on ipsilateral molars, splaying was produced along the inferior border of the angle of mandible in a model in the single miniplate technique.
Brons and Boering (1970), inventors of the lag-screw system highlighted the possibility for primary bone healing. If the screws are aligned in a position perpendicular to the fracture line the fracture segments are forced together, resulting in primary bone healing. Here, the main difference between the miniplate and lag-screw methods is obvious.12 It is generally accepted that reduction and fixation of the fracture to align the fragments in contact promotes bone healing. Moreover, a direct correlation between the fracture-gap width and the healing process is given in the literature; if the fracture-gap width is larger than 2 mm, then bone healing is delayed. Large fracture gaps cause a delay in fracture healing, as demonstrated in experimental and clinical investigations. A good reduction of a fracture with small inter-fragmentary gap is important for its revascularization and healing.8
The study done by Edward Ellis III and Walker showed that single miniplate used for treating non-comminuted fractures of the mandibular angle. They observed a gap along the inferior border of the mandible in some of the patients on immediate post-operative radiographs and there was no clinical malocclusion and by the 6th week post-operative radiograph the gap had completely closed.12 Similar observations were found in our study where, mean fracture gap preoperatively in Group 1 and Group 2 was found to be 1.91mm and 1.82 mm respectively. In the immediate post-operative period fracture gap was reduced to 1.28 mm and 1.18 mm respectively and at the 8th week follow-up stage the gap was completely obliterated. Since the gap between fracture fragments was less than 2 mm, likely chances of delayed union or nonunion is not excepted because most of authors viewed that increased gap between fracture fragments in the range around 4mm can invite complications such as nonunion and delayed union.8, 12
Conclusion
Considering the results of our study, we conclude that the lag screw fixation has all the advantages over miniplate fixation. The clinical outcomes of both the lag screw system and standard miniplate systems in the present study were similar. However, the following advantages with the use of lag screw can be highlighted like Relatively lesser fixation time, Superior fracture fragment stability, fewer complications, Stable occlusion & less hardware, less cost required. Though lag screw in our study is giving promising results, it has not reflected in terms of statistical significance because of fewer numbers of cases. Therefore, subjecting a large sample size of patients treated with the technique of lag screw for the management of fracture fixation at angle region would yield specific critical values to substantiate our observations.