- Visibility 18 Views
- Downloads 4 Downloads
- DOI 10.18231/j.jsas.2023.023
-
CrossMark
- Citation
Excisional arthroplasty of hip for complex periprosthetic fracture: A case report
Introduction
Girdlestone Excisional Arthroplasty (GEA) first described by Girdlestone has been used frequently as a salvage procedure for painful hip joints due to tuberculosis.[1] It leads to painless mobile hip but causes shortening and instability.[2] The procedure involves excision of head and neck of femur and maintaining gap between the hip and the basal part of neck by heavy traction for 8 to 12 weeks leading to a long fibrous ankylosis permitting good range of movement. The procedure is less undertaken these days due to evolution of better surgical technique of total joint replacement, prevention of infection as a result of improved perioperative asepsis, skilled steps of surgery with less tissue trauma and effective antibiotics. Conversion of GEA to a Total Hip Replacement/Arthroplasty (THR/THA) is possible but there remains strong possibility of reinfection and dislocation.[3] Despite THR, GEA has an important role in salvaging infected total hip arthroplasty cases or cases where revision surgery has failed or there is problem of unmanageable periprosthetic fracture. GEA is considered an effective method of eradicating infection and alleviating pain in such cases.[4] The case report herein describes periprosthetic fracture in a case of bipolar arthroplasty where GEA was accepted as the preferred procedure and resulted in satisfactory result.
Case Report
A 36 years old male grocery shop owner by profession was admitted in orthopedic ward of tertiary care hospital in the central India with the chief complaints of pain and difficulty in walking and weight bearing on the right lower limb for 2 months. The patient had slipped at home on the right lower limb after which he felt pain in the right upper thigh. He was not able to stand and walk after the fall. He was operated 14 years back in 2009 for an injury in the right hip area. The femur head was replaced in that surgery and patient had recovered fully within a few weeks and carried his daily activities without any limitation till he had the trauma 2 months back. No documentation was available regarding the previous fracture and the surgery. He was not a known case of diabetes or hypertension.
On examination the patient was of average built with normal vital parameters and systemic examination did not show any abnormality. His weight was 81 kg., height 162 cm and BMI 30.86. Inspection revealed external rotation of the right lower limb, diffuse swelling in proximal half of right thigh and shortening of about 3 cm. There was healed scar of posterior approach to the hip. Right femur upper shaft was tender and felt thickened on the posterolateral aspect. Abnormal mobility was demonstrable in this area. No active movements of the hip were possible. The passive movements were full but terminally painful. X-ray pelvis AP view ([Figure 1]) showed fractured bipolar prosthesis on the right side. There was fracture in the upper fourth of shaft right femur along with fracture through the mid part of stem of the prosthesis. The fractures were transverse and the proximal fragment was abducted with total loss of contact between the fragments. The head of prosthesis inside the bigger cup was well seated and the prosthesis head was in normal alignment with the acetabulum. The case was diagnosed as Periprosthetic fracture right femur and management plan considered was prosthesis removal followed by THR. The difficulties of prosthesis removal were anticipated as it was cemented prosthesis along with the fracture both of stem and the shaft femur. The possibility of leaving the gap unconstructed (excisional arthroplasty) was also considered and the patient was explained all complications, treatment options and prognosis. Informed written consent was taken.
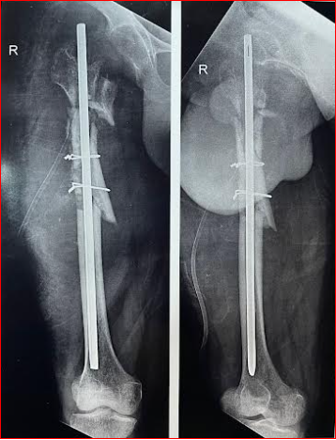
The patient was taken in left lateral position after spinal anesthesia. A 15 cm long oblique incision was made along the old scar. Through the lower most part of the incision the shaft femur distal to the fracture was approached. A window of 1.5x 1.5 cm was made just distal to the tip of the prosthesis stem and attempt was made to push proximally the broken stem by hammering from below over a curved punch and pulling from proximal site. On its failure, the distal stem was removed after doing vertical osteotomy of femur along the window upwards. During removal of the bone cement by curette the fragments got comminuted and were splinted by a cerclage wire. Next the head of prosthesis and its remaining stem was also removed with difficulty only after vertical osteotomy of the proximal fragment. The bone had become comminuted in this process and it was considered not fit for any type of arthroplasty. A Kuntchner’s nail (K nail) of 36 cm length and 9 mm diameter was inserted in from greater trochanter downwards to maintain length and rotation of the limb and thus accepting excisional arthroplasty. The limb was kept in skeletal traction by upper tibial Steinmann pin for 8 weeks with quadriceps strengthening and joint mobilization exercises. The wound healed uneventfully. The postoperative x-rays ([Figure 2]) showed reasonably aligned femur with fractured fragments splinted with 2 cerclage wires and K nail in position. The patient gained good range of hip movements. He was kept non weight bearing for total 12 weeks and then started ambulation initially with walker and later with stick. At the last follow up his hip was painless and thigh was non tender, and the limb length was 1 cm short. Hip flexion was 0 to 100 degrees, extension 0 to 20 degrees, abduction 0 to 40 degrees, adduction 0 to 20 degrees and both internal and external rotation 0 to 20 degrees. The patient was walking with stick and managing his daily work without any difficulty. His x-ray thigh showed fragments in acceptable position and uniting phase. He continues to remain under follow up.

Discussion
Periprosthetic fractures are fractures around joint replacement prostheses. These fractures include fractures of parts of the prosthesis with or without fractures of the bone, commonly femur. Fractures of femur with THR are common and require optimal treatment. Periprosthetic fractures are seen more frequently due to increased number of joint replacement surgery being done in aging population in hip, knee, shoulder and elbow. Treatment of these fractures pose new challenge to orthopedic surgeons. High failure rate and mortality are reported in these cases.[5]
Periprosthetic fractures have been classified as per Vancouver classification by Duncan[6] in type A, B and C depending on the location of the fracture. Type A fractures occur within proximal metaphyseal area. It is subtyped as AG, when the fracture is around greater trochanter and AL, when the fracture is around lesser trochanter. Type B fractures occur at or just below the tip of the femoral prosthesis. These are further subtyped as B1, fracture around a well fixed prosthesis, B2, fracture where prosthesis is loose but bone stock is good and B3, fracture where prosthesis component is loose and there is good osteolysis and bone loss. Type C periprosthetic fractures occur well distal to the femoral stem. Epidemiology and treatment of periprosthetic fractures associated with THR have been studied by various authors.[6], [7] Periprosthetic fracture was first reported in 1954.[8] Incidence of periprosthetic fracture is reported to be 4.1%, with increasing rates for uncemented and revision THA cases.[9], [10] Late periprosthetic fractures have been noted to be the 3rd most common cause of revision surgery after aseptic loosening and infection.[11] Mean time of fracture after surgery has been noted to be 7.4 years and 3.9 years respectively in primary and revision THA cases.[10] High activity level is also noted as a predisposing factor in young adults.[12]
The reported case underwent Bipolar Prosthetic Replacement at the age of 22 years for a complex fracture of neck Right femur. He was doing normal activities after that for 14 years without any symptoms. A fall in home caused the periprosthetic fracture for which he was referred to our center. The fracture radiologically can be categorized as type AL, as it is below the lesser trochanter through the mid part of the femoral stem. The ideal management should have been prosthesis removal and total hip arthroplasty. Per operative difficult prosthesis removal and comminution of femur in the shaft and trochanteric area made us abandon THA option and accept the excisional arthroplasty as the best option for the patient. Skeletal traction with active hip mobilization for 8 weeks followed by non- weight bearing for further 4 weeks resulted in a painless, mobile and near normal long limb and a satisfied patient.
Conclusion
Excisional arthroplasty of hip is a practical option in treatment of cases of complex periprosthetic fractures leading to failure of revision surgery.
Source of Funding
None.
Conflict of Interest
There is no conflict of interest of any author.
References
- FT Robert Horan. Gathorne Girdlestone and excision arthroplasty of the hip. J Bone Joint Surg Br 2005. [Google Scholar]
- S Kessler. Extensive subtrochanteric shortening osteotomy enables the conversion of a long lasting resection arthroplasty to a total hip replacement. Acta Chir Orthop Traumatol Cech 2008. [Google Scholar]
- WPH Charlton, PH William. Complications associated with reimplantation after girdlestone arthroplasty. Clin Orthop Relat Res 1976. [Google Scholar]
- R Vaishya, V Vijay, A Vaish. Successful salvage of an unstable Girdlestone's excision arthroplasty with a megaprosthesis of the hip. J Clin Orthop Trauma 2015. [Google Scholar]
- A Capone. Periprosthetic fractures: epidemiology and current treatment. Clin Cases Mineral Bone Metab 2017. [Google Scholar]
- CP Duncan. Fractures of the femur after hip replacement. Instr Course Lect 1995. [Google Scholar]
- D Marsland, SC Mears. A review of periprosthetic femoral fractures associated with total hip arthroplasty. . Geriatr Orthop Surg Rehabil 2012. [Google Scholar]
- IB Horwitz, MI Lenobel. Artificial hip prosthesis in acute and nonunion fractures of the femoral neck: follow-up study of seventy cases. J Am Med Assoc 1954. [Google Scholar]
- DJ Berry. Epidemiology: hip and knee. Orthop Clin North Am 1999. [Google Scholar]
- H Lindahl, H Malchau, P Herberts, G Garellick. Periprosthetic femoral fractures: classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthrop 2005. [Google Scholar]
- H Lindahl, G Garellick, H Regnér, P Herberts, H Malchau. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am 2006. [Google Scholar]
- D J Berry. Periprosthetic fractures associated with osteolysis: a problem on the rise. J Arthroplasty 2003. [Google Scholar]
