Introduction
For more than fifty years, anterior cervical discectomy and fusion (ACDF) has been a widely accepted operation for cervical spine degenerative diseases, including disc herniation and spondylosis, that are refractory to medical management. The high rates of success and patients’ satisfaction with ACDF has made the operation a standard of care in common neurosurgical practice, however, the advantages of cervical disc arthroplasty (CDA) over fusion including maintaining normal neck motion and reducing degeneration of adjacent segments of the cervical spine.3 In the literature, CDA results are at least similar or even superior to clinical outcomes after anterior cervical arthrodesis at short- and medium-term follow-up.The implantation of CDA was reported to be a safe procedure, However, despite the low revision rates, favorable outcomes, feasibility, and ability to perform explanation of artificial disc prostheses,many surgeons still have negative perceptions of cervical arthroplasty. No study that we are aware of has compared the adjacent-level reoperation rates for CDA versus the natural history of the disease. Furthermore, we believe that other significant factors limiting the more widespread use of CDA include the technical difficulty of the procedure compared to ACDF, complications such as spontaneous fusion and loosening, postoperative hematoma, heterotopic ossification (HO) and, in some countries, decreased reimbursement compared to ACDF.Moreover these reports have proven that CDA devices can maintain segmental mobility at the indexed level(s) and likely have the potential to reduce adjacent segment disease (ASD). 1
This paper is a review of the current literature, to determine the radiological and clinical outcomes of patients who underwent CDA for cervical degenerative disease and to compare with widely used ACDF procedure in cases of cervical myelopathy this in order to help inform preoperative decision-making and discussions with patients.
Materials and Methods
Inclusion & exclusion criteria
Consecutive adult patients (> 18 years of age) who underwent one- or two-level CDA with Prestige LP artificial discs (Medtronic, Memphis, TN) at the subaxial (C3–7) cervical spine in a single institute were included. The surgical indication for CDA was symptomatic cervical disc herniation and/or spondylosis causing radiculopathy, myelopathy, or both, that was refractory to medical treatment. All patients had failed at least 12 weeks of non-operative management, including physical and pain control therapy, but remained medically intractable prior to surgery.
Exclusion criteria were
Spinal trauma and fracture;1, 2 evident segmental instability (i.e. more than 3.5mm translation or 20° angular motion); 3 arthrodesis without mobility;4 severely incompetent facet joints;5 adjacent segment disease;6 ossification of posterior longitudinal ligament (OPLL);7 kyphotic deformity;8 infection; and9 long-term steroid use
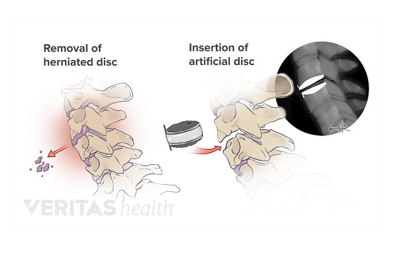
Surgical technique
The standard Cloward approach for anterior cervical discectomy was executed in all patients. In addition to thorough discectomy, bilateral uncovertebral joints and bone spurs were removed extensively with drilling burrs or Kerrison’s rongeurs to achieve generous decompression of the dura sac and nerve roots. Also, the posterior longitudinal ligaments were always resected to ensure adequate decompression. Upon placement of the Prestige LP artificial disc, meticulous endplate preparation, selection of a proper fitting size, and centering of the device were considered imperative to minimize the chances of heterotopic ossification (HO) formation. 2 Furthermore, we used copious saline irrigation persistently to wash away the bone dust generated from osteophyte drilling in every case. All surgeries were done by three experienced neurosurgeons (JC Wu, WC Huang, and H Cheng) with consistent techniques detailed in our previous publications. 3, 4, 5, 6, 7, 8
Clinical and radiological follow up
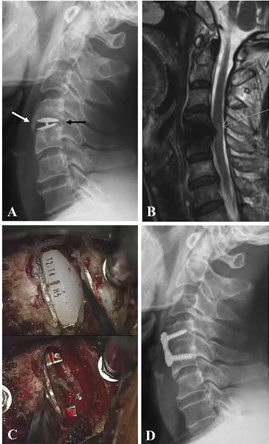
Regular visits at the outpatient department were arranged at pre-operation, and post-operative 6-weeks, and at 3, 6, 12 and 24months for all patients. Clinical follow-up parameters included visual analog scales (VAS), neck disability index (NDI), and modified Japanese Orthopaedic Association (JOA) scores, which were collected by experienced physician assistants during regular post-operative follow-ups. Routine X-ray images including antero-posterior, lateral, and flexion-extension films were taken at every regular visit at the clinic. Radiological criteria for adjacent segment degeneration (ASD) in X-ray films were the presence of disc space narrowing, osteophytes, or sclerosis of the endplates. 9 Incidences of HO formation were accessed by not only the post-operative lateral radiographs but also by CT scans with three-dimensional reconstruction, and graded according to the McAfee’s classification. 10 Segmental range of motion (ROM) at the index level was Page 3 of 9 determined with standing lateral flexion/extension radiographs (Figure 1) at post-operative 24-months follow-up using the Cobb method.2 Radiological measurements were completed by a board-certified neuroradiologist independently using the PACS system software, SmartIris (Taiwan Electronic Data Processing Co., Taiwan).
Observation and Results
A total of 171 patients underwent 1- or 2- level CDA with Prestige LP artificial discs, with an average age of 48.3±9.99 years at the time of operation. In order to investigate the age-related effects of CDA, the current study aimed to analyze patients at the two ends of the age distribution in the cohort. Therefore, the study included 71 patients who were aged 65 years or more and those less than 40 (to a minimum of 18years), to minimize the bias from mid-aged CDA patients. The demographic data of these are demonstrated in Table 1. The patients were divided into two groups: the elderly group (≥65years old) consisted of 24 patients with a mean age of 71.2±4.79years; the young group (≤40years) composed of 47 patients with a mean age at 33.9±4.45 year-old. The mean follow-up duration was 28.0 months, without differences between the two groups (averaged 22.6 versus 30.8 months, elderly vs. Young, respectively). The most commonly indexed levels of CDA were C4–5 and C5–6, accounting for 85%of the entire series. Approximately 50 min, consumed for the CDA surgery in the two age groups. The clinical outcomes, including VAS of neck and arm pain, NDI, and JOA scores were all similarly satisfactory after the surgery, during the follow-up. All the patient-reported outcome parameters had significant improvement at the final follow-up, when compared to the pre-operative scores(Table 2).
Table 1
Demographic data
Table 2
Clinical outcomes
Discussion
The current study focused on acomparison of patients at both ends of the age distribution (≧65or≤40years) in a cohort of CDA patients. Patients who had been followed-up for more than 24 months were included for retrospective analysis of their clinical outcomes(i.e. VAS,NDI, and JOA scores), radiological parameters(i.e. pre-,post-operative ROM, and incidences of HO), and the complication profiles (e.g.dysphagia,dysphonia, and C5palsy). The study demonstrated small but distinct discrepancies between the elderly and young in the changes of segmental mobility after CDA. More than 2 years after 1-or 2-level surgery for CDA, both groups of patients, regardless of their age differences(i.e. elderly versus young),demonstrated improvements in clinical outcomes when compared to that of pre-operation. Moreover, both groups had successfully preserved segmental mobility at the indexed levels with CDA. comparing different prostheses with ACDF or between the various types of prostheses is reasonable. The clinical application of the Discover cervical artificial disc was first reported by Greiner–Perth et al. 11 in 2009. Discover prosthesis is both a metal-on-polymer type and a non-constrained type of prosthesis, which may have advantages in terms of the incidence of heterotopic ossification and ASD.
In our study, the postoperative neck disability index (NDI) and VAS scores of both the ACDF group and the TDR group were significantly improved from their preoperative scores, and there was no significant difference between the two groups at different time points (up to at least a two-year follow-up). Published randomised controlled clinical studies have shown the non-inferiority of short-term outcomes of TDR surgery compared to ACDF surgery. 12, 13, 14 We similarly did not find a significant difference in overall complication rates due to adjacent segment degeneration between the two procedures at a mean of 5.4 years of follow-up across both groups.
Veeravagu et al.15 reviewed 28,777 cases undergoing ACDF and found that 9.13% of the single-level and 10.7% of the multilevel ACDF groups required a second operation within two years. They reported that the number of fusion levels was significantly correlated with the rate of reoperations. At 48 months, Davis et al.16 reported a cumulative incidence of 4% reoperation at the index level in the TDR group.
As more research is conducted on artificial disc replacements and surgical techniques continue to improve, it is likely that ADR will become an even more important part of spine care in the future. For patients suffering from back pain or other spinal conditions, ADR offers a safe and effective alternative to traditional spinal surgery that can help them regain their mobility and quality of life.
This recent study highlights the benefits of cervical disc arthroplasty and reinforces the importance of considering all options when deciding on a treatment plan for cervical disc disease. Patients should discuss their individual needs and the risks and benefits of ADR with a board-certified physician to determine if it is right for them.
Conclusion
There are numerous benefits to CDAs. Cervical arthroplasty can mitigate pain and neck disability in appropriate patients with degenerative cervical disc disease causing radiculopathy or myelopathy. CDAs has been demonstrated to preserve segmental motion at long-term followup and to decrease the incidence of adjacent-level surgery, as compared to ACDF. Cervical global alignment and the segmental angle at rest improves after cervical arthroplasty. Onthe other hand, there are also some negatives associated with CDA. It is not appropriate for anyone with osteoporosis, ossifying diseases, instability, collapsed disc, facet arthrosis, inflammatory diseases, spinal infections and retro vertebral disease. It is also technically demanding to implant a perfectly sized, perfectly placed prosthesis and there are numerous pitfalls that can result in poor outcomes. Despite the challenges, when performed technically well in appropriate patients, we believe that cervical arthroplasty is a safe and effective alternative to anterior cervical arthrodesis with several potential benefits.