Introduction
Dirofilariasis is categorised under the group of parasitic infections caused by filarial nematodes belonging to the genus Dirofilaria (Nematoda, Filarioidea, Onchocercidae). 1 Various species under this genus include Dirofilaria repens, Dirofilaria immitis, Dirofilaria tenuis and Dirofilaria ursi. 2, 3, 4 D. repens primarily infects the subcutaneous tissue of dogs, foxes, and cats, while D. immitis inhabits the right ventricle and pulmonary artery of dogs and cats. 1
Many European nations have recorded cases of human dirofilariasis caused by Dirofilaria repens. Sri Lanka is the most impacted nation in Asia, with a canine infection rate of about 60%.5 Inflammatory subcutaneous nodules caused by the worm in exposed areas such as the face, orbits, upper limb, lower limb, chest wall, and male genitalia are the most typical presentation of the disease. 6
The vectors for this parasite include Adult female Culex, Aedes and Anopheles mosquitoes. The microfilaria are ingested by the vectors as they take the blood meal of an infected host. The third stage larva of microfilaria develops in the Malpighian tubules of mosquitoes before migrating through the body cavity to the proboscis. When an infected mosquito bites the dogs or other hosts, such as humans, during a subsequent blood meal, disease transmission occurs.7, 8
Case Report
A 44-year-old lady presented with left neck pain of 2 weeks duration. On examination, a 2 x 2 cm swelling with tenderness was noted in the upper 1/3rd of the left sternocleidomastoid muscle (Figure 1). The ultrasonography disclosed a nodular lesion measuring 10.4 x 6.7 x 6.9 mm in the upper part of the left sternocleidomastoid muscle with alive moving dirofilarial worms(Figure 2).
Figure 2
USG showing a nodular lesion measuring 10.4 x 6.7 x 6.9 mm in the upper part of left sternocleidomastoid muscle with moving Dirofilarial worms.
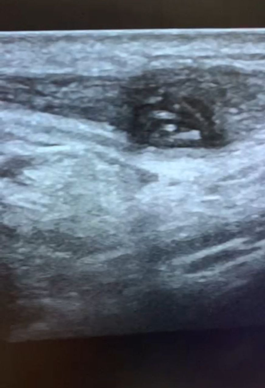
Figure 4
a; and b; showing cross section of the Dirofilarial worm surrounded by mixed inflammatory infiltrates
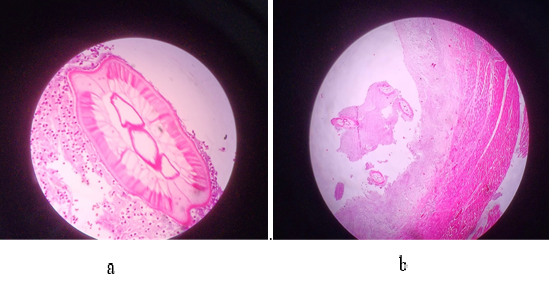
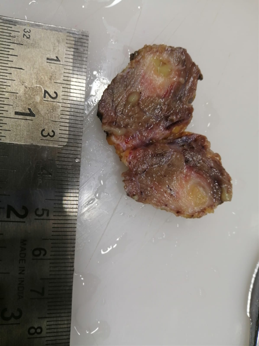
Surgical excision of the swelling was performed under general anesthesia (GA). A cross sectional examination of the biopsy specimen showed a tiny cystic cavity measuring 5 mm in greatest dimension, and containing a worm measuring 0.5 cm in length (Figure 3). Microscopy revealed sections of skeletal muscle with a cystic cavity containing cross sections of a worm, morphology resembling that of Dirofilaria repens and surrounded by mixed inflammatory infiltrate (Figure 4 a and b), thus confirming the diagnosis of intramuscular Dirofilariasis.
The patient was started on anti-helminthics post-operatively and successfully discharged on the 3rd postoperative day.
Discussion
Human dirofilariasis can be divided into pulmonary dirofilariasis (D. immitis) and subcutaneous dirofilariasis (D. repens, D. tenuis, and others). Subcutaneous and submucosal lesions are the symptoms that are most frequently observed.3
According to the open-access literature, between 30 and 60 percent of canines in various parts of the nation are affected, and mosquitoes like Aedes aegypti, Armigeres subalbatus, Mansonia uniformis, and Mansonia annulifera are the vectors that are involved in transmitting the disease.3, 5, 8 Since humans are not the natural hosts of Dirofilarial worms but rather accidental dead-end hosts, it is found that the infectious larvae injected by mosquito bites in humans fail to attain full maturity and hence cannot express larvae in the bloodstream, which explains the rarity of human microfilaremia. Dirofilariasis cannot be spread from person to person since its natural mode of transmission involves microfilariae, which in no way infect humans.9 Anti-filarial/anthelmintic drugs are ineffective in the majority of the documented cases because there are no microfilariae in the blood stream.5 As a result, the treatment that is a combination of complete excision of the nodule and worm extraction is observed to be usually successful. In the literature, surgical excision and parasite isolation are more frequently presented as primary diagnostic and therapeutic approach at the same time. In the instance being discussed, the primary diagnostic technique was ultrasound, which is a fairly reliable way to identify subcutaneous filariasis. Although the parasitological and patho-histological analyses are necessary for the final confirmation of the diagnosis, ultrasound scan can also very confidently resolve the differential diagnosis of the subcutaneous nodule.
Conclusion
Although the number of human infections with D. repens has been rising in tropical regions, many of them remain undiagnosed or unreported. Due to the presence of disease-transmission vectors, this could result in a sudden outbreak of this particular disease. In order to decrease the prevalence of this disease through controlling vector densities, accurate diagnosis and patient care, there is a need for the acquisition of greater knowledge of this infection, diagnostic procedures and vector control methods.