Introduction
Fingertip amputations are commonly seen in children due to door crush injuries. Reconstruction of the fingertip is needed to maintain the finger length, sensation of the tip and cosmesis.1, 2, 3 There are various methods described for reconstructing fingertip amputations.4, 5 We present a case of Allen type IV amputation of the right ring finger which has been reconstructed with cross finger flap along with nail bed graft.
Case Presentation
6 year old child was brought to emergency room 1.5 hours following amputation of the right ring finger following door crush injuries. On examination there was Allen type 4 oblique amputation of the right ring finger with exposed distal phalanx and profuse bleeding. There was loss of nail plate, nail bed and pulp tissue. Child was anxious and in pain. Movements at the proximal interphalangeal joint of the ring finger are normal. X ray revealed amputation at the level of distal phalanx. Amputated part was examined which consisted the nail bed, part of the distal phalanx and pulp tissue. The neurovascular bundle was found to be crushed and avulsed.
Treatment
The right ring finger was thoroughly debrided. Retained part of distal phalanx was exposed with total loss of sterile matrix. Germinal matrix was found avulsed. It was re-inserted.
To improve the cosmesis, sterile nail bed graft of size 1 cm x 1 cm was harvested from the amputated part and sutured on to the remains of germinal matrix. Following this cross finger flap was designed and raised from the dorsum of the middle finger. Flap inset was done into the defect. Split thickness skin graft harvested from the medial aspect of the forearm to resurface the defect on the dorsum of the middle finger. An above elbow cast was applied following the procedure. After 2 weeks the flap was divided and inset done. Physiotherapy was started after the flap division and child achieved complete flexion of ring and middle finger at the end of 3 weeks.
Discussion
Finger amputation in children beyond the lunula have been routinely managed closure of the stump, composite tissue graft, homodigital flaps, heterodigital flaps, regional flaps, distant flaps and replantation. Replantations have become the primary choice for fingertip reconstruction for amputation till the level of lunula if vessels are reparable. It is technically challenging and failure may happen in severe crush injuries. Replantation restores the normal function and anatomy6, 7, 8 but the duration of procedure is lengthy, needs microscope and specialized post-operative care with prolonged hospital stay and cost.
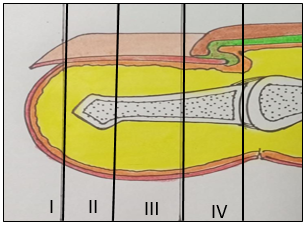
Allen has classified fingertip injuries into four types.2 Type I involves only the pulp of the finger. Type II includes pulp and nail bed. In type III there is partial loss of distal phalanx along with part of pulp and nail bed. Type IV involves the lunula, pulp, nail bed and terminal phalanx.
Cross finger flap was first described by Gurdin in 1950 and Pangman in 1951.9 Since then it has been widely used to cover the volar defects of distal and middle phalanx of fingers.
The rectangular flap is elevated from the dorsal aspect of the middle phalanx. The base of the flap is on the neutral line of the donor finger which is usually adjacent to the injured finger. The flap is raised superficial to the paratenon of the extensor tendon.
Blood supply to the flap is from the dorsal branch of the digital vessels. The flap is then inset into the defect and donor finger defect is resurfaced with split thickness or full thickness skin graft.
Cross finger flap is easy to perform, reliable with minimal donor site morbidity. Disadvantage is it being a 2 staged procedure; first stage the flap inset is done and second stage the flap is divided. Cross finger flap is reliable and effective in preserving the length, restoration of cosmetic appearance and providing sensibility.
Nail aids in improving the stability and sensibility of the pulp. It also improves the cosmesis of the fingertip.10, 4 Free nail bed grafts help in increasing the nail length thus making the finger more cosmetically pleasing. Graft repositioning includes thorough debridement of the amputated stump, separation of full thickness nail bed from amputated distal phalanx and suturing it over the remnant proximal distal phalanx.11 In this procedure graft which is non-vascularised gets nutrition from the plasmatic fluid. The revascularisation begins after 72 hours. After imbibition of the flap new blood vessels grow into the graft.
In our case the ring finger was amputated obliquely at the level of lunula. The neurovascular bundle was avulsed with loss of nail bed. Hence we decided to maintain the available length with cross finger flap. To reconstruct the nail and give the finger near normal cosmesis we decided to harvest the nail bed graft from the amputated part. The graft survived on the flap and showed nail growth of 6.4 mm.
Conclusion
We conclude that cross finger flap and nail bed graft gives excellent result in Allen type 4 amputation of fingertip. The cosmesis is near normal with good flexion at the DIP joint. There is also 7 mm visible nail plate which adds to stability of the distal phalanx. The technique of harvesting the nail bed and repositioning over the distal phalanx along with cross finger flap is reliable and can be easily executed in such cases.