Introduction
Over 70 years have passed since insulin was recognized as crucial for wound healing.1 While substantial evidence supports its benefits, no suitable administration method for routine clinical use has been established. Systemic insulin is limited due to significant side effects, while topical insulin struggles with reliable delivery. Research shows varying topical doses, and insulin receptors are found in many tissues, suggesting effective local application could enhance healing if concentrations are maintained.2 This study tests the hypothesis that local insulin injections can sustain high concentrations in wounds, promoting healing with minimal systemic effects while combining the advantages of systemic and topical approaches.
Case Report
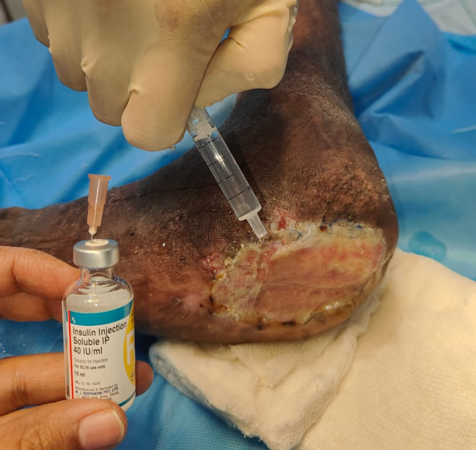
This study was conducted in the Department of Plastic Surgery at a tertiary care centre in South India. The patient was a 69-year-old male with a history of left diabetic foot with Charcot’s joint with a non-healing ulcer over the lateral aspect of left foot.
To enhance healing at the donor site, the area was irrigated with a combination of Insulin Isophane and Human Insulin (70/30) in a ratio of 4 units of insulin mixed with 10 ml of 0.9% normal saline per 10 cm² of area. Following this, a two-layer regenerative scaffold dressing was applied, along with Negative Pressure Wound Therapy (NPWT) to support optimal recovery.
Results
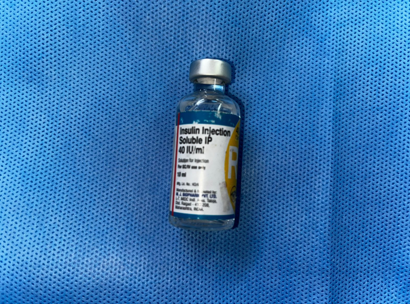
The application of insulin enhances the healing process by promoting keratinocyte migration and differentiation, as well as angiogenesis, ultimately leading to a reduction in healing duration.(Figure 1, Figure 2, Figure 3)
Discussion
Wound healing is a complex and dynamic process that involves the reconstruction of cellular structures and tissue layers.3 It can be divided into three primary stages:
Inflammatory Phase: This initial phase involves the recruitment of blood cells, such as macrophages and neutrophils, which help to clear debris and fight infection.
Proliferative Phase: Here, the focus shifts to tissue formation, including the production of extracellular matrix and new blood vessels, leading to the development of granulation tissue.
Remodeling Phase: In this final phase, the newly formed tissue matures and strengthens, improving the integrity of the wound.
Effective wound healing relies on the coordinated action of various proteins, genes, and cellular mediators.4
Wound bed preparation, encapsulated by the acronym T.I.M.E5,, aims to optimize the healing environment for chronic wounds:T: Tissue—assessing and managing non-viable or deficient tissue.I: Infection/Inflammation—addressing and controlling infection.M: Moisture Balance—ensuring an appropriate moisture level in the wound.E: Edge—focusing on the wound edge to promote granulation tissue growth.
Recent literature has highlighted the use of topical insulin as a promising approach in wound bed preparation, potentially enhancing healing outcomes in difficult-to-heal wounds.6 Topical insulin enhances wound healing by modulating oxidative stress and inflammatory responses.7 Research shows that insulin treatment reduces levels of reactive oxygen species, which can have harmful effects on lipids, proteins, and DNA in burn wounds in animal models. 8 Moreover, topical insulin promotes the early recruitment of neutrophils and exerts an anti-inflammatory effect by increasing the number of M2 macrophages and levels of IL-10, aiding in the clearance of dead tissue.9 In vitro studies demonstrate that insulin enhances macrophage chemotaxis and phagocytosis while regulating the expression of MCP-1 at wound sites.10 In addition to its effects on inflammation and re-epithelialization, topical insulin promotes keratinocyte migration, accelerates re-epithelialization, and stimulates fibroblast activity.11 The mechanisms behind insulin-induced keratinocyte migration and differentiation rely on insulin receptors, but also involve epidermal growth factor receptors (EGFR), mediated through the PI3K-Akt-Rac1 signalling pathway.12 Treatment with topical insulin on burned skin has been shown to improve collagen deposition and maturation, indicated by increased levels of hydroxyproline.
Beyond regulating inflammatory and re-epithelialization processes, insulin also promotes angiogenesis in wounds. Topical insulin increases the formation of new blood vessels in healing tissues, and subcutaneous insulin injections have been linked to enhanced migration of microvascular endothelial cells and the formation of endothelial tubes. These effects are associated with the PI3K-Akt-SREBP1 signalling pathway.13 Additionally, there is increasing evidence that topical insulin has pro-angiogenic effects and aids in vessel maturation in diabetic wounds, likely by restoring impaired insulin signaling pathways, such as PI3K/Akt and MAPK/ERK, and enhancing the expression of VEGF and angiopoietin-1.14 Various types of wound dressings are available that facilitate healing through the controlled and sustained release of bioactive insulin, further contributing to the recognition of topical insulin in wound healing. However, additional research is necessary to deepen our understanding of insulin's role in healing different types of wounds. These are limitations of our study.
Conclusion
Topical insulin significantly improves wound healing by targeting inflammation, re-epithelialization, and angiogenesis. As its application in wound management continues to gain recognition, further research is essential to elucidate the mechanisms of action and assess its efficacy across different wound types.